- Breakthrough For Ehlers Danlos Syndrome and Endometriosis - 13 March 2025
- Does EDS get worse as you age? - 20 February 2025
- Can Ehlers Danlos Syndrome Cause Weight Gain/Loss? - 18 February 2025
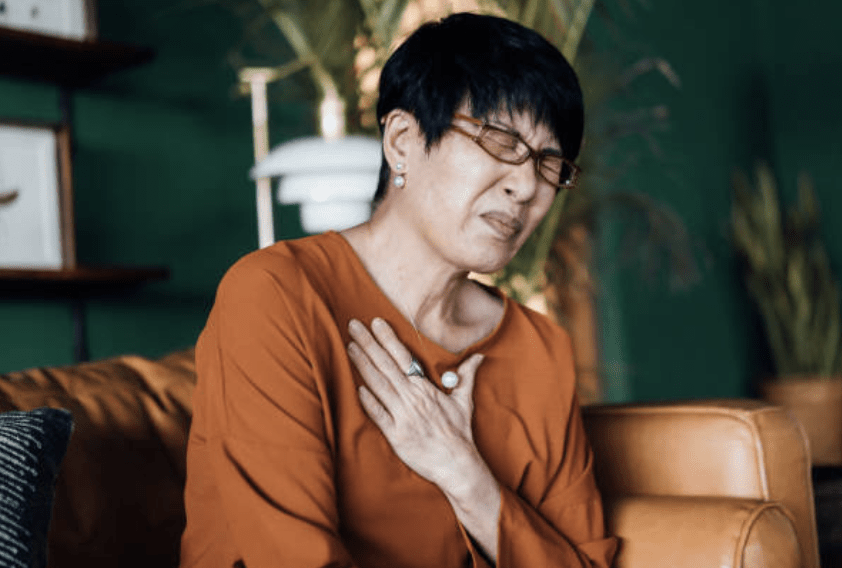
Fibromyalgia and Costochondritis are two conditions that often go hand in hand with each other. Over the years we have lost count of the number of clients who were plagued with the hallmark sharp stabbing pains, that often come with Costochondritis. Within this topic are many questions, most of which become a whole lot harder to answer when we factor In Fibromyalgia.
There are many people in the general population who have Costochondritis, it’s not just another issue that comes along with Fibromyalgia. However, as we will come to find when we take a look at some of the research, Costochondritis does seem to be far more prevalent in those with Fibromyalgia.
This article covers:
ToggleWhat is Costochondritis?
Costochondritis is the term given to inflammation of the cartilage that joins your ribs to your breastbone, also known as the costochondral joint. Inflammation is a natural response to illness or injury, it’s essentially the immune system’s response to help initiate the healing process, in other words, it is a defence mechanism that is vital to our survival.
Whilst Inflammation is one of the body’s greatest tools, it doesn’t feel all that great when it does happen. After all, the point of inflammation is healing, and this means that more blood is redirected to the area, tissues become more permeable to allow increased blood flow and nutrients to the areas, and the nerves in the surrounding areas become a whole lot more sensitive. If you have ever had a paper cut you will know exactly what I mean. For such a small cut, it sure does impact your day to day activities.
With Costochondritis, the costochondral cartilage, which connects your ribs to your breastbone, and surrounding tissue can become inflamed, making it tender and unpleasant when pressure is applied, and in most cases, simply from breathing or even moving.
Symptoms of Costochondritis
The obvious leading symptom is chest pain, typically it is described as a sharp or stabbing pain, and sometimes it is described as more of a dull ache which often becomes worse when moving or exerting the chest muscles. This can also include breathing, which can cause an increase in pain with large breaths. Many people find that even the slightest touch or pressure around the sternum and ribs can fire off a pain response, as the nerve becomes more and more sensitive due to the inflammatory response.
The most commonly reported pain from Costochondritis can be found in the sternum, around the 4th-6th ribs. However, as the inflammation increases, it’s not uncommon for the pain to begin to spread.
Does Costochondritis cause fatigue?
A question we hear a lot of is “Does Costochondritis cause fatigue?”
Again, this question takes a little research and some critical thinking to answer. There are some good studies that show us that there is a pretty strong connection between fatigue and Rheumatic conditions in general. In one study of patients with different rheumatic conditions, there was found a 54% prevalence of fatigue for those with a single inflammatory rheumatic disease, such as rheumatoid arthritis, systemic lupus erythematosus, or ankylosing spondylitis. However, this prevalence shot up to 82% for those with Fibromyalgia. In essence, from this and multiple other studies, one out of every two patients with a rheumatic disease seems to be severely fatigued.
On one side of the coin, there are many folk in the general population who do have Costochondritis but report minimal fatigue. And on the other side of the coin, we have those with fibromyalgia and Costochondritis, who report major fatigue associated with it. It’s unlikely that costochondritis directly causes fatigue, as both those with fibromyalgia and without it would be affected. However, that does not mean that it does not indirectly cause fatigue.
If you ask anyone with chronic pain about sleep, they will tell you that it’s incredibly difficult to get a good nights sleep when you are in pain. And one of the hallmark symptoms of sleep disturbances and deprivations is fatigue. Therefore, it’s not such a huge leap to assume that someone with Costochondritis, or Fibromyalgia and Costochondritis, would experience fatigue as an indirect result of being unable to sleep properly due to being in pain.
Likewise, many people with Fibromyalgia, often learn and develop certain coping skills for sleeping when it comes to dealing with the pain of Fibromyalgia. It’s very likely that due to differences in the pain experience, Costochondritis may cause undue stress and anxiety which could disrupt sleep also. Pain from Costochondritis is very hallmarked, it’s sharp, disruptive, and can often make people wonder if there is something wrong with their heart. Therefore, many people with Fibromyalgia and Costochondritis may struggle to sleep due to the new pain that comes from Costochondritis.
Is there a connection between Fibromyalgia and Costochondritis
When living with Fibromyalgia, it is often hard to distinguish what pain comes from which issue. Many people have gone to their doctors with legitimate concerns, only for those concerns to be passed off as just another Fibro symptom.
One example of this is from a consultation we had here at The Fibro Guy, some years back. A young woman had been suffering from severe headaches and every time she went back to the doctors it was promptly put down as caused by Fibromyalgia. However, at her consultation with us, and after going through her history, it was blatant that this young woman had Ehlers-Danlos syndrome. What also stood out was that her headaches were immediately cut in severity when she lay down. Suspecting a Cerebrospinal fluid leak we quickly referred her to her local hospital. And low and behold, it was indeed a spinal fluid leak. After a blood patch, and bed rest to closely monitor for leak recurrence, she recovered after around 6 weeks and has never had another headache since.
We have many stories from over the years just like this one, but the point to take is that you should never put new symptoms down to Fibromyalgia.
While working with our clients in the studio, it’s really not uncommon for us to get the “Is my Costochondritis and Fibromyalgia related?” question. And this is a good question, anecdotally you probably know a whole host of individuals with Fibromyalgia and Costochondritis, but are they related.
When looking at the evidence on this topic, it becomes more clear that they are likely linked, as the prevalence of patients with Fibromyalgia who also have non-cardiac chest pain is far higher than in the general population. In a study conducted in 2016 that looked at symptoms of people with Fibromyalgia, across 4 groups it was found that on average, 29.1% of the 313 participants either currently or previously had Costochondritis. And when compared to the general population, it was found that chest pain in primary care it only accounted for 13%.
In an overview of symptoms of patients hospitalised in the US between 1999-2007, there were over 1.7 million people during this time with Fibromyalgia, of those patients, 10% presented with non-specific chest pain (around 170,000 people). While this is closer to the general population we have to remember that these were only the ones who felt the pain was bad enough to go to the hospital, and its worth remembering that when living with Fibromyalgia, it tends to take a much higher level of pain before seeking medical intervention due to living in pain being accepted as normal.
There may well be a few reasons why are more commonly found together:
- Sleep
If the last few decades of research into sleep and pain have taught us anything, it’s that with lack of sleep comes a prevalence for more pain. Sleep disruptions lead to hyperalgesia pain changes, which means that your brain becomes far more responsive to noxious stimuli, lowering the pain threshold, and even going as far as to impact your own body’s ability to realise pain-killing chemicals. For those with fibromyalgia, sleep is most often a major issue. Therefore, an activity that would not normally be deemed as strenuous, may become strenuous for someone with Fibromyalgia, and could potentially lead to the development of Costochondritis, due to inflammatory responses from strenuous activity or movement. - Guarding response
For those in pain, it’s really not uncommon to find them adopting postures to make the pain more bearable. Whilst this may help in the short term, over time staying in any one position can become painful. In the instance of Costochondritis, it’s not a far reach to assume that putting prolonged strain on the costochondral joints and cartilage, could potentially cause an inflammatory response causing Costochondritis for those with Fibromyalgia. - Lack of activity
The decrease in activity levels amongst those with Fibromyalgia, as well as being in pain, can lead to sensitisation which lowers tissue tolerance to stress before an inflammatory response is deemed necessary. For tissue to be healthy, we need to move, and for those with Fibromyalgia, this can often be an issue. This gives us another potential reason for a link between Fibromylagia and Costochondritis. - Hypermobility
It has been shown in a number of studies that there is a link between hypermobility and Fibromyalgia. One study showed that 46.6% of the Fibromyalgia patients participating, scored at least 4 or more on the Beighton scoring system (A method used to determine hypermobility), compared to 28.8% of the control group. When we look deeper at the connection between Fibromyalgia and Hypermobility, the issues surrounding chest pain and Fibromyalgia can be further explained.The high prevalence of misdiagnosis in the hypermobile population most likely contributes to the increase of those with Fibromyalgia experiencing inflammation of the chest. A common symptom surrounding hypermobility, is that of joint subluxation/dislocation, due to the genetic make-up of collagen. And a common issue associated with this is rib subluxation. We wrote an article about hypermobility rib subluxation earlier this year, which you can find here. Hypermobility may account for the prevalence of Costochondritis in the Fibromyalgia population, as slipping rib syndrome is pain from inflammation of the cartilage that
Fibromyalgia Chest Pain
Chest pain can be terrifying when it happens, it can even be severe enough to mimic the symptoms of a heart attack. I remember when I had my first experience of this, I actually thought I was dying and it wasn’t until I was in the hospital, that I found out that I was fine. But, nonetheless it was a pretty scary experience, as I couldn’t breathe properly because of the pain, and it felt like a tight band around my chest.
The good news though, is that Costochondritis is it is not cardiac-related, so it isn’t related to the heart. When there is inflammation in the chest this often leads to shortness of breath, due to us trying to breathe in a more limited fashion to reduce the pressure on the chest. This change in our respiration will often lead to us not taking in as much oxygen as we normally would, and can leave us feeling like we can’t breathe and panicked. But, again, Costochondritis is it is not cardiac-related.
Can Fibromyalgia make Costochondritis worse?
Living with Fibromyalgia is bad enough, but when adding Costochondritis to the mix it can seem a whole lot worse. But can Fibromyalgia make Costochondritis worse?
Fibromyalgia often leads to central and peripheral sensitization where nerves are a lot more sensitive to noxious stimuli, so it will take less pressure on the chest before these nerves fire and alert the brain of a potentially dangerous stimulus. This would make it feel a lot more tender to the touch than it should normally be. Think of a turn dial that usually likes to sit at 1-3 unless something is wrong (like inflammation) and is then turned up when there is an issue. With Fibromyalgia though, the dial is already sitting at 7, so when a potential threat is noticed this can turn it up to 10. This can result in more painful sensations than are usually warranted. So, given what we know about the current pain mechanisms, having fibromyalgia is likely to make having Costochondritis worse than it would be for someone without fibro.
Treating Costochondritis or Fibromyalgia chest pain
Your first port of call when it comes to Fibromyalgia and Costochondritis should be your doctor. Anti-inflammatories will help to deal with a lot of the pain from Costochondritis, but this isn’t a long term solution. As we previously mentioned, having a healthy and happy rib cage means that it needs to be able to move freely, so this should be your second port of call: focusing on relearning to move your ribs.
We would also suggest that you check to make sure that you are indeed not Hypermobile and that the pain doesn’t arise from a rib subluxation. In either case, we have some gentle exercises designed to open up the rib cage and turn down sensitivity, in the video below.
We hope you enjoyed ready!
— The Fibro Guy Team —
Looking for more articles on Fibromyalgia?
Read our blog on Fibromyalgia and Osteoarthritis
Read our blog on Fibromyalgia headaches
Enjoyed Our Blog? Why Stop Here?
If you’ve found value in our posts, imagine the impact of a structured, science-backed course tailored specifically for fibromyalgia and its unique challenges. The Full Body Fibro Course is your ultimate starting point for understanding your body, improving mobility, and managing symptoms effectively.