- POTS and Exercise: The First Step Everyone Misses - 27 June 2025
- The Missing Link Between Breathlessness, Fatigue, and Chronic Pain: Understanding CO₂ Tolerance - 19 June 2025
- What is Mast Cell Activation Syndrome? - 12 May 2025
Please click below if you would prefer to listen to this article on EDS and hypermobility flare-ups.
Many people often say that Hypermobility/ Ehlers-Danlos Syndrome is the gift that keeps giving. Unfortunately, it just so happens that the gifts it gives so readily do so in the form of EDS flare-ups, pain, and multiple systemic issues!
While everyone feels differently about which issues feel the worst, most agree that the constant flare-up of symptoms is at least in the top three. So, today, let’s look at flare-ups: what they are, why they happen, and, more importantly, what we can do about them.
This article covers:
ToggleWhat is an EDS flare-up?
EDS flare-ups are essentially a sudden intensification of symptoms, and that’s probably the best way to define them. However, they can vary widely from person to person because EDS affects connective tissue, which is essentially the body’s glue that’s virtually everywhere. This means that a flare-up can feel like a systemic meltdown, affecting everything from the cardiovascular system to the gastrointestinal tract, and even coat hanger pain.
Additionally, it means that an EDS flare-up will be very subjective from person to person due to the systemic nature of issues that connective tissue disorder brings about. For some, a flare-up might mean a sharp increase in gastrointestinal issues; for others, it may be an increase in dizziness and pain due to comorbidities like Postural Tachycardia Syndrome (PoTS). However, for many folks, it may be all of the above plus subluxations or dislocations.
When we break it down, an EDS flare-up is a temporary increase of symptoms in one or more systemic issues accompanying Ehlers-Danlos syndrome.
What causes a flare-up?
Now, as you are probably starting to understand, flare-ups can be very nuanced because collagen is everywhere. This means that for some people with issues like dysautonomia, factors like heat, physical strain, and dehydration can be the main drivers of their flare-ups.
For others, with perhaps the vascular type of EDS, which is characterised by more fragile blood vessels and organs, a flare-up could be due to injury or being knocked into, which could lead to more severe complications, such as ruptures or bruising.
The most common type of EDS is the hypermobile type, and a flare-up can be triggered by factors ranging from a sudden increase in activity, injury, or even psychosocial stressors. As you likely know already, this subtype is notorious not just for its joint instability issues but also for a spectrum of secondary conditions like gastrointestinal disturbances, autonomic dysregulation (such as POTS), mast cell activation syndrome (MCAS), and chronic fatigue, all of which can have the propensity to drive flare-ups of their respective symptoms, and very often others.
So, here is a quick overview of the question of what can cause a flare-up for those with EDS; it depends on the type of EDS you have and which systemic issue is driving it:
- For those with dysautonomia, factors like heat, physical strain, and dehydration can exacerbate symptoms.
- In cases of MCAS, potential triggers from medications, all the way to environmental antigens like pollens, certain foods in their diet, perfumes, and even stress events can lead to flare-ups.
- Similarly, for those suffering from ME/CFS, post-exertional malaise is a hallmark symptom, and overexertion can worsen their condition.
- Hormonal fluctuations also play a significant role, as evidenced by some studies where individuals have reported a worsening of symptoms during hormonal changes such as the perimenstrual or post-partum periods.
- Stress, too, is a common trigger that can exacerbate EDS symptoms, potentially due to its effects on the nervous system and inflammation levels.
Whilst the cause of a flare-up is going to be nuanced, certain factors will likely cause a flare-up for most with EDS, and these include:
Sleep Disturbances
The relationship between sleep disturbances and pain has been widely studied, largely showing that with sleep disturbances comes an increase in pain. It is not only well established that poor sleep directly causes more pain but also a sharp decline in physical functioning and mood, especially during the early parts of the next day.
Moreover, one small survey of EDS patients in 2001 showed increased difficulties with sleep in the population. It was estimated that of those with EDS, 56% had difficulty maintaining sleep. So, you are not alone. Sleep problems have become almost a staple of Ehlers-Danlos syndrome and hypermobility, which means they can be a big driver behind flare-ups.
Gastric issues
Another driver of flare-ups for many people is gastric issues, especially conditions like Gastroesophageal reflux disease (GERD), which occurs when stomach acid repeatedly flows back into the tube connecting your mouth and stomach (oesophagus). This backwash (acid reflux) can irritate the lining of your oesophagus. GERD has been well documented in those with hypermobility and EDS, often prevalent in upwards of 50% of the population in some studies. I can personally attest to this one, which is one of the reasons why I no longer eat late at night: It’s just not worth it.
The main reason, however, that this can drive flare-ups is because of how it affects sleep. Most people think they understand how important sleep is, but most have no idea how important it is. This is one of the reasons we write this comprehensive article on sleep. Additionally, a comprehensive study from Norway revealed that individuals experiencing both insomnia and GERD symptoms were three times more likely to report disturbances during the night than those without sleep issues. As we discussed earlier, sleep disturbance causes pain flare-ups.
Irritable Bowel Syndrome (IBS)
This is notably prevalent among individuals with Hypermobile Ehlers-Danlos Syndrome, which affects up to 62% of patients. This overlap between IBS and EDS complicates the diagnosis and management of these conditions. Unlike individuals who experience IBS without hypermobility, those with hypermobility and EDS face unique challenges due to the systemic nature of their condition, which complicates standard IBS treatment protocols.
IBS flare-ups often involve significant abdominal pain and discomfort, which can increase the body’s stress levels, leading to chronic stress. Chronic stress is known to exacerbate the symptoms of EDS, such as joint pain and fatigue. Likewise, increased IB symptoms can affect nutrient absorption and digestion, leading to poor nutrition, weakening the body’s overall health, and impacting collagen synthesis, muscle strength, and energy levels.
Research has shown that nearly all individuals (98%) diagnosed with a hypermobility spectrum disorder also meet the criteria for Adult Functional Gastrointestinal Disorders (FGIDs). This overwhelming crossover suggests that the gastrointestinal symptoms may be more severe, frequent, or difficult to manage than those experienced by individuals with IBS alone, meaning they can be a very big potential driver of EDS flare-ups.
Hormonal Changes
Hormonal fluctuations are likely to drive flare-ups, particularly due to the increased laxity they can cause in connective tissues. This is most noticeable in individuals experiencing natural menstrual cycles, where certain phases, such as the luteal phase, can drastically increase symptoms.
In the 10-14 days leading up to menstruation, levels of progesterone increase, which can enhance the laxity of connective tissues. This heightened laxity can result in more frequent and severe subluxations and dislocations, as well as intensifying pain and fatigue, due to a decrease in GABBA, leading to a notable flare-up of overall EDS symptoms. Another thing to note in these areas is the effect of hormonal contraceptives such as birth control pills (BCPs) and hormonal intrauterine devices (IUDs), which alter the natural hormone cycles. These contraceptives typically suppress the cyclical peaks and troughs of oestrogen and progesterone that are natural to the menstrual cycle, leading to what is known as a pill bleed rather than a true period. This artificial regulation of hormones can mask the natural triggers of EDS flare-ups, complicating the management of the syndrome.
What does an EDS Flare-Ups feel like??
When a flare-up strikes, it’s like an existential storm that overtakes the body without warning, leaving a trail of diverse and intense symptoms in its wake, such as:
Physical Sensations:
The pain experienced during a flare-up can be excruciating and multifaceted. Some describe it as a deep, gnawing muscle pain that feels like someone is relentlessly twisting a screwdriver into the limbs. This pain isn’t stationary; it can migrate from one part of the body to another, such as from the elbow to the leg, intensifying to the point where it becomes unbearable.
Others report experiencing “fire skin,” where patches of skin emit a burning sensation so severe it feels like being held against a flame. This peculiar symptom can appear suddenly and linger, excruciating even the lightest touch or the brush of clothing.
Joint and Muscle Challenges:
You already know that joint instability is a hallmark of EDS. During a flare-up, this can lead to an increase in subluxations or dislocations with minimal provocation as the cortical maps blur. This not only contributes to the pain but also adds a layer of psychological distress, as one must be constantly vigilant to avoid movements that could potentially trigger a dislocation.
Muscle spasms are also fairly common. Some describe them as feeling as if their muscles are cramping or seizing up, even when they are not actively using them. This sensation can be so severe that it feels like the muscles are vacuum-sealed, pulling tighter with no relief.
Systemic and Neurological Symptoms:
Flare-ups often bring a suite of systemic symptoms, including debilitating headaches, which might manifest as intense, head-splitting pain that comes and goes unpredictably. Neurological symptoms during a flare include heightened sensitivity to pain, where even a gentle scratch can reverberate deep into the muscles and bones, causing severe discomfort.
The fatigue associated with EDS flare-ups is profound and pervasive. It’s more than just feeling tired; it’s a comprehensive exhaustion that compromises cognitive function, making even simple tasks feel monumental. Some describe it as soul-sucking fatigue and a disorienting fog that clouds their thoughts and judgment.
Emotional Impact:
The unpredictability and intensity of flare-ups exert a significant emotional toll. The constant pain and fatigue can lead to feelings of isolation and frustration as routine activities and social engagements become increasingly difficult. The chronic nature of these symptoms can also stir feelings of anxiety and depression as individuals grapple with the unpredictability of their condition and the impact it has on their quality of life.
Avoiding and Managing EDS Flare-Ups
This is the part you have probably been waiting for or skipped. If you did, then I don’t blame you. Flare-ups can be hard and affect almost every area of your life. However, what I want you to take away from this section is that avoiding flare-ups or managing them when they happen comes down to you and the Biopsychosocial factors that govern your health.
What I mean by this is not to think of EDS in general; think individually. You have already seen so far that flare-ups come down to many interlinking factors, such as sleep affecting the stomach or temperature affecting POTS. So, If you have issues with mast cells and histamine, and your current diet seems to be putting you in a flare, reach out to a dietitian, look at the FOD map diet, and ultimately try and mitigate the biggest contributing factors to your flare up if they are diet base. We wrote a huge comprehensive article on hypermobility and diet with EDS dietitian and expert Katie Mednick, which you can find here.
This includes monitoring your osmotic balance, especially if dealing with PoTS alongside EDS. Managing fluid intake with isotonic drinks can help maintain proper hydration levels and prevent shifts in your body’s osmotic pressure that might trigger a flare-up. Staying hydrated with the right kind of fluids is crucial to your overall health, particularly in managing the symptoms of these conditions. Postural Orthostatic Tachycardia, in some studies, is an independent predictive factor for GI dysmotility; this alone shows you how flare-ups come down to many interlinking parts.
This is easier said than done, but it ultimately pays dividends. Triggers, though, are not created equal, and while you may have some control over the foods you eat, you don’t have any control over the weather. So, a sudden increase in temperature as summer approaches means that issues like PoTS may get very bad if you don’t have a plan to mitigate them.
For those more sensitive to triggers like joints moving out of place, pulling on ligaments, and causing a flare-up in pain, proper conditioning and cortical mapping training are needed to help stabilise joints. We wrote a compressive article on this subject; you can find it here in the hypermobility part 1 article.
In essence, avoiding flare-ups comes down to understanding how EDS affects you as an individual and putting plans into place to either stop the driving factors causing your EDS flare-ups or mitigate them as much as possible. Some of these factors, like the weather, will be out of your control, but many of them, my friends, are within your control, and that’s what it’s about: being proactive to avoid the many pitfalls that come with EDS, including flare-ups.
Please feel free to check out our Hypermobility resource section for help addressing some of the drivers of your own flare-ups.
-Adam-
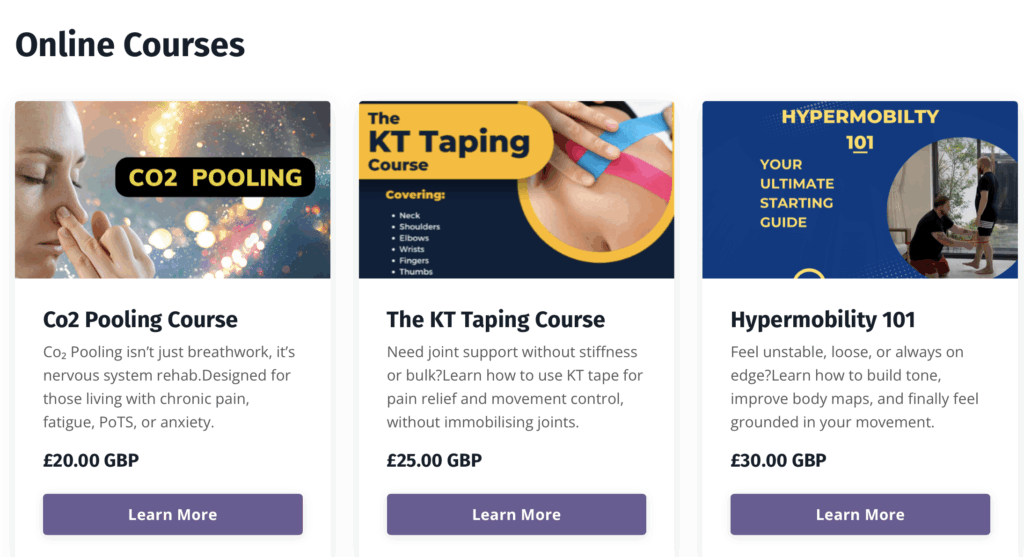
Enjoying Our Resources? Why Stop Here?
If you’ve found value in our posts, imagine what you’ll gain from a structured, science-backed course designed just for you. Hypermobility 101is your ultimate starting point for building strength, stability, and confidence in your body.
FAQ: Common Questions About EDS Flare-Ups
What does an EDS flare-up feel like?
A “body-wide escalation of symptoms” is one way to describe an EDS flare-up, in which a number of symptoms—including but not limited to: joint pain, exhaustion, vertigo, and gastrointestinal problems—gain intensity. It impacts numerous bodily systems at once and varies in intensity, but it usually feels overwhelming.
How long can a EDS flare-ups last?
A flare-up of Ehlers-Danlos Syndrome (EDS) can last anything from a few days to a few weeks, though this varies greatly from person to person. The intensity of symptoms is a factor that determines how long a flare-up lasts; symptoms that are more severe tend to last longer. The length of time a flare-up lasts can be influenced by various factors, including specific triggers like exercise, stress, or illness. Recovery time can also be affected by how well management strategies, such as medication and physical therapy, work. While some people with EDS may feel better after a flare-up, others may have symptoms that last for a long time and need constant care and attention.
What can I do to prevent EDS flare-ups?
Pacing oneself, eating right, drinking enough of water, getting enough sleep, and strengthening one’s supporting muscles with light, frequent exercise are all part of a comprehensive prevention plan. One must be aware of their own triggers in order to prevent or lessen the severity of flare-ups.




