- POTS and Exercise: The First Step Everyone Misses - 27 June 2025
- The Missing Link Between Breathlessness, Fatigue, and Chronic Pain: Understanding CO₂ Tolerance - 19 June 2025
- What is Mast Cell Activation Syndrome? - 12 May 2025
Many people think of fibromyalgia as an invisible disease. It is characterised by pervasive pain, constant tiredness, and the aggravating haze of mental difficulties. Low blood pressure, however, is an indicator that is under-recognized. Most people don’t realise how deeply it is linked to fibromyalgia.
Interestingly, hypermobility is frequently misdiagnosed as fibromyalgia. This condition, characterised by unusually lax connective tissue, shares many overlapping symptoms with fibromyalgia. Hypermobility often coexists with low blood pressure, creating a challenging mix of symptoms that can feel nearly impossible to untangle.
Feeling dizzy on standing up, overly tired even after resting, or confused by your symptoms? You’re not alone. Many people feel ignored or disregarded because the links between fibromyalgia, low blood pressure, and sometimes hypermobility are seldom clarified.
This blog will analyse the research findings regarding fibromyalgia and hypotension. Most importantly, we will provide you with practical strategies to manage these interrelated symptoms, and we will also discuss the role of hypermobility.
This article covers:
ToggleThe Link Between Fibromyalgia and Low Blood Pressure
We usually picture chronic pain and extreme exhaustion when we consider fibromyalgia symptoms. However, hypotension, which is less talked about, is surprisingly common in fibromyalgia patients. To get to the bottom of this, we need to examine the autonomic nervous system (ANS), a major regulator in the human body.
Your body’s automatic processes, such as digestion, temperature regulation, blood pressure, and heart rate, are under the control of the autonomic nervous system. In essence, it ensures that everything is functioning properly without your intervention. Fibromyalgia, however, frequently causes this system to malfunction.
Abnormal blood pressure responses are common among fibromyalgia patients, particularly when the patient must make rapid adjustments, such as when they stand up from a seated or lying down position.
Tilt table tests are used to assess the body’s ability to control blood pressure; however, research indicates that as many as 60% of fibromyalgia patients report substantial drops in blood pressure during these tests.
On the other hand, nobody in the healthy control group exhibited these behaviours.
Instability, vertigo, lightheadedness, and fainting spells are all symptoms of low blood pressure.
In addition to making everyday tasks more difficult, these symptoms can cause anxiety when standing up or moving too fast, which further restricts mobility and independence.
Autonomic nervous system dysfunction isn’t haphazard. It appears to originate from the same abnormalities in the nervous system that cause the other symptoms of fibromyalgia, including increased tiredness and pain. Basically, the nervous system’s ability to regulate blood pressure can be compromised when it’s overloaded.
Circadian Blood Pressure Patterns
Circadian rhythms are innate to the human body and help regulate a number of functions, including the day-to-night changes in blood pressure. The majority of people’s blood pressure naturally drops while they sleep, which gives their bodies a chance to recharge, fix, and get ready for the next day. But this crucial process frequently fails in fibromyalgia.
As a general rule, blood pressure typically drops by 10–20% while we sleep. As a whole, your health and recovery will benefit from this dip because it gives your cardiovascular system a break.
The nocturnal dip in blood pressure is less pronounced or nonexistent in fibromyalgia patients, according to the research. Scientifically speaking, this pattern is called a “non-dipping” pattern.
The rejuvenating effects of sleep are diminished when blood pressure does not drop as it ought to during the night. People may find themselves even more drowsy, sleepy, and unmotivated upon waking as a result of this disturbance.
Tiredness isn’t the only thing that the non-dipping pattern addresses. Additionally, it has been associated to elevated levels of inflammation and cardiovascular strain, two major issues for fibromyalgia patients.
Some fibromyalgia sufferers report feeling faint or lightheaded first thing in the morning, even before getting out of bed, which may be due to their inability to properly regulate their blood pressure while they sleep.
Why Hypermobility Adds Complexity
Our main emphasis is on fibromyalgia, but we must not overlook the high frequency of hypermobility as a symptom of this condition. There is a connection here that can make symptom management harder and, at times, even more perplexing; it’s not a mere coincidence.
Based on Beighton scores, research indicates that hypermobility is present in 46% to 81% of fibromyalgia patients. In clinical settings, that overlap is frequently disregarded, despite its significance.
Hypermobility goes beyond mere flexibility, as more than just the joints are affected by this systemic issue. Controlling blood vessels is one of its most noticeable effects. Hypermobile folk typically have trouble constricting their blood vessels, which causes poor circulation, blood pooling in the legs, and unsteady regulation of blood pressure.
The already prevalent symptoms of fibromyalgia, such as dizziness, lightheadedness, and chronic fatigue, can take on additional forms due to these problems. Managing hypermobility and fibromyalgia symptoms simultaneously can be al be incredibly challenging.
The fact that some fibromyalgia patients experience non-responsive persistent vertigo or fainting spells is also explained by this overlap. Not only is fibromyalgia a factor, but hypermobility is further complicating matters.
Making sense of this link isn’t merely for the benefit of academia. It’s an important first step in receiving the help you need. Healthcare providers can better address both conditions when they recognise hypermobility in fibromyalgia patients.
Managing Fibromyalgia with Low Blood Pressure
It takes a multi-pronged strategy that takes neurological and physical aspects into account to manage fibromyalgia and low blood pressure. There isn’t a silver bullet, but there are several evidence-based approaches that we can take thanks to research that can help us tackle these interrelated problems.
Medications, lifestyle changes, and dietary strategies are all part of the toolbox when it comes to helping with fibromyalgia symptoms and blood pressure regulation.
Pharmacological Interventions
Low blood pressure is a common complication of fibromyalgia, and medications can help with both symptoms and the condition. Medication cannot eliminate all symptoms, but it can alleviate some of the most debilitating ones, such as vertigo, exhaustion, and chronic pain, greatly enhancing quality of life. To make sure these treatments are safe, effective, and customised to your needs, ensure work closely with your healthcare provider.
Propranolol:
It is common practice to prescribe the beta-blocker propranolol to patients suffering from hypertension, migraines, or specific cardiac conditions. Clinical trials are still in the early stages of determining its efficacy in the treatment of fibromyalgia.
In fibromyalgia, autonomic dysfunction causes a decrease in blood pressure, but early pilot trials show that propranolol may help regulate this drop. Patients with fibromyalgia often experience sympathetic nervous system overactivity; this treatment may help alleviate this condition.
Caveats: Although preliminary results show promise, larger-scale clinical trials are required to establish its complete effectiveness and safety for fibromyalgia patients in the long run.
Ideal for: People whose vertigo, irregular heartbeat, or other symptoms intensify when they’re under emotional or physical strain.
Propranolol isn’t right for everyone; it can aggravate asthma and cause heart problems in some people. Fatigue, chilly extremities, and low blood sugar levels are some of the possible side effects, especially for diabetics.
Amitriptyline
Pharmacological treatment of fibromyalgia has long relied on amitriptyline, a tricyclic antidepressant. It works wonders at low doses for pain, insomnia, and blood flow problems.
An increase in the brain’s serotonin and norepinephrine levels is how amitriptyline gets its analgesic effects. Improving the quality of sleep is an important part of managing fibromyalgia, whilst also having a mild sedative effect.
Blood pressure benefits: Improving blood flow to affected tissues at low doses (about 10-25 mg daily) can alleviate symptoms of poor circulation and low blood pressure. The results of the research indicate that amitriptyline can help fibromyalgia patients sleep better, feel less pain, and have better physical function generally.
Ideal for: People who have trouble sleeping, experience generalised pain, or have symptoms that might be worsened by low blood pressure.
Things to keep in mind: Amitriptyline has the potential to induce side effects like increased appetite, lethargy, constipation, and dry mouth. It is crucial to carefully manage dosages because higher doses might disrupt autonomic nervous system function.
Midodrine and Fludrocortisone
Orthostatic hypotension, a rapid decrease in blood pressure upon standing, is a common symptom of fibromyalgia patients experiencing autonomic dysfunction; these two medications are mainly prescribed to treat this condition.
The synthetic corticosteroid fludrocortisone increases sodium retention in the kidneys, which is how it works. Because of this, blood volume increases, which aids in maintaining a steady blood pressure.
Advantages: It can lessen the likelihood of dizziness, increase energy, and prevent low blood pressure suddenly.
Cons: Fluid retention, hypertension, and electrolyte imbalances are long-term side effects that need close monitoring.
In contrast, the alpha-agonist medicine midodrine works by making the blood vessels constrict, which in turn raises blood pressure as the patient stands up from a seated position.
Advantages: It can lessen orthostatic hypotension-induced vertigo and lightheadedness.
Cons: You might experience tingling, itching on the scalp, or goosebumps as side effects. Due to the risk of dangerously high blood pressure while lying down, midodrine should not be taken at night.
People whose autonomic nervous system malfunction causes them to faint or experience dizziness on a regular basis may benefit the most.
Both drugs necessitate constant vigilance over electrolyte and blood pressure levels. They are usually prescribed as a part of a larger treatment program that also involves changes to one’s way of life.
Some Other Important Medications
Reuptake Inhibitors of Serotonin and Norepinephrine (SNRIs):
In order to alleviate both the pain and the mood symptoms associated with fibromyalgia, doctors may recommend medications such as Venlafaxine (Effexor) and Duloxetine (Cymbalta).
Pregabalin, brand name Lyrica, is a common medication for fibromyalgia nerve pain. Although it has no effect on blood pressure per se, it does alleviate symptoms such as lightheadedness and sensitivity to pain.
Key Point: Medications Fit Within a broader Context
Because of these individual differences, there is no “magic bullet” when it comes to medication. Although they can alleviate symptoms to a certain extent, they work best when combined with other treatments, such as those that encourage physical exercise, behavioural modifications, and stress reduction techniques.
Prior to beginning or changing any medication, it is imperative that you consult with your healthcare provider.
Lifestyle Modifications
When it comes to managing fibromyalgia and low blood pressure, lifestyle changes are often the most overlooked yet powerful tools in your symptom management toolkit. While they might seem simple, these adjustments can have a profound impact on your energy levels, circulation, and overall well-being.
Hydration and Salt Intake
Although it may sound simplistic, controlling salt intake and maintaining adequate hydration can significantly impact blood pressure stabilisation and alleviate symptoms such as dizziness and exhaustion.
Drink two to two and a half litres of fluids every day. The stability of your blood pressure depends on your blood volume, which you can keep steady by drinking enough of water. If you feel lightheaded when you stand up, it might help to drink some water before switching positions. Hypertension can be transiently increased by as little as one glass of water.
Add salt to your diet in moderate amounts, but make sure to consult a doctor first. Because it aids in fluid retention, salt can help regulate blood pressure, however, this isn’t about seasoning everything with salt. Soups, electrolyte drinks, or lightly salted snacks are better options for adding small, deliberate amounts.
As a quick tip: have a refillable water bottle on hand and set an alarm to remind you to drink water at regular intervals throughout the day. It’s surprisingly easy to neglect getting enough water when symptoms are at their worst.
Exercise
There has always been some ambiguity in the relationship between exercise and fibromyalgia, and its something we have wrote about in great depth. Avoiding movement altogether can exacerbate stiffness, poor circulation, and low energy, while doing too much too soon can trigger flare-ups. The ideal situation calls for gradual, low-impact movements that you can intensify as your fitness level rises.
Benefits of Exercise for Low Blood Pressure:
- Improved Cardiovascular Function: Regular physical activity strengthens the heart and improves circulation, which can help stabilize blood pressure levels. Studies have shown that individuals who exercise consistently exhibit better cardiovascular health compared to those who are sedentary.
- Resistance Training: Both low-speed and high-speed resistance training improve muscle strength and overall physical performance. While these interventions might not directly change blood pressure levels, they play an important role in supporting overall physical stability and reducing symptom severity.
- Aerobic Exercise: Activities such as brisk walking, cycling, or light swimming have been linked to better blood pressure regulation. Aerobic exercise enhances circulation, which may help reduce dizziness and fatigue.
- Managing Symptoms: Regular, light to moderate physical activity can improve circulation, reduce blood pooling in the lower extremities, and minimize symptoms like dizziness and fatigue.
Practical Tips for Exercise with Fibromyalgia and Low Blood Pressure:
- Start with gentle activities like walking, yoga, or tai chi. These exercises are kind to your joints and improve circulation without overwhelming your system.
- Move slowly and intentionally. Avoid sudden changes in position, such as jumping up from sitting to standing, as these can trigger dizziness.
- Incorporate resistance exercises with light weights or resistance bands, focusing on controlled movements rather than speed or intensity.
- Pay attention to how your body responds. If you start to feel dizzy, fatigued, or lightheaded, stop and rest.
Regular movement isn’t just about physical health. It also boosts mood, enhances sleep quality, and reduces overall symptom intensity.
Compression Garments
Although compression garments aren’t exactly a show-stopper, they are a lifesaver for those suffering from low blood pressure or blood pooling.
The gentle squeezing action of compression stockings or tights aids in preventing blood from collecting in the legs. When you’re standing or changing positions, this easy trick can help alleviate symptoms like lightheadedness and dizziness.
If you’re looking for compression stockings, try to find a pair with graduated tightness that loosens up the leg as you go up the leg. In most cases, these are better for blood circulation. Even though knee-high compression stockings don’t provide the same level of support as full-length ones, they can still be quite helpful.
Although the effects of making changes to one’s lifestyle may not be immediately apparent, they can be powerful and endure for a long time. Supporting your body’s natural systems with hydration, gentle movement, and compression garments establishes a more solid groundwork for your health.
It’s fine to begin modestly. Perhaps it’s taking an additional glass of water first thing in the morning, stretching for five minutes before going to sleep, or using compression socks on days when vertigo is particularly bad. The most important thing is to form routines that you can actually stick to.
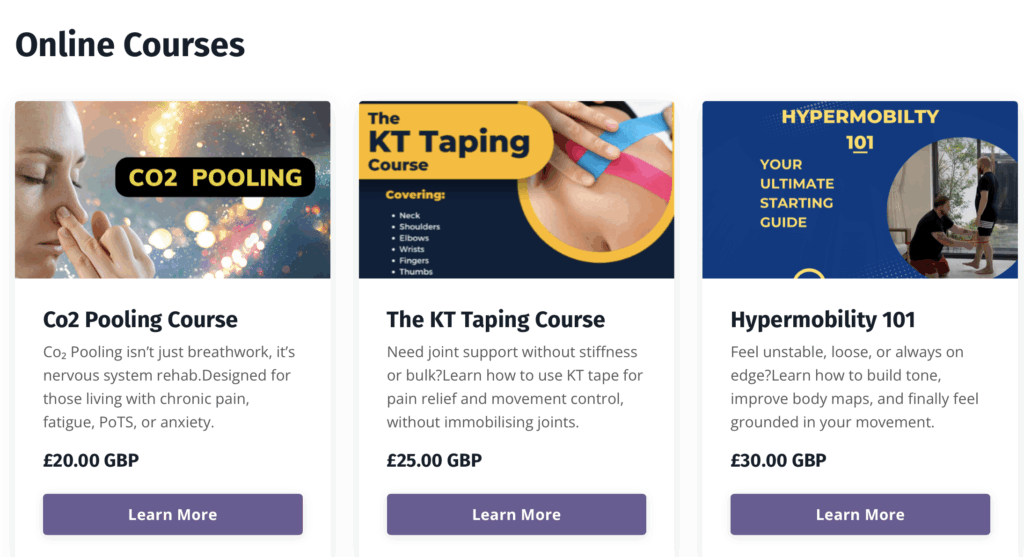
Enjoyed Our Blog? Why Stop Here?
If you’ve found value in our posts, imagine the impact of a structured, science-backed course tailored specifically for fibromyalgia and its unique challenges. The Full Body Fibro Course is your ultimate starting point for understanding your body, improving mobility, and managing symptoms effectively.