- Breakthrough For Ehlers Danlos Syndrome and Endometriosis - 13 March 2025
- Does EDS get worse as you age? - 20 February 2025
- Can Ehlers Danlos Syndrome Cause Weight Gain/Loss? - 18 February 2025
If you would prefer to listen to this article, then please click below.
Every once in a while we get a client that comes through the door with both Fibromyalgia and sciatica. Unfortunately, for many people with Fibromyalgia, most new symptoms get put down to simply yet another Fibro symptom. However, if you do have Sciatica, then you will likely already know, that sciatica pain feels very different to normal everyday Fibromyalgia pain.
So, with that being said, I am going to say the same thing to you at home reading this, as we do to our clients in the studio: Do not put symptoms down to Fibromyalgia.
Sciatica is the loose term for one type of lumbar radiculopathy, essentially meaning pain and other symptoms, caused by irritation of a lumbar nerve root or at least a part of it. It’s also good to keep in mind that sciatica is a symptom, rather than a specific diagnosis, and not a particularly specific one either. The term sciatica can be rather confusing, with many medical professionals using it to describe radiculopathy involving the lower extremities and relating to herniated disks. And many patients refer to sciatica as any pain that shoots down the legs.
Now, for anyone with Fibromyalgia, adding sciatica into the mix can make an already painful day, into a seemingly impossible task! However, the good news though, is that most cases of sciatica will resolve on their own within 6 weeks, without the need for any special intervention or treatment.
Most people will never have this problem again, and the rest perhaps a few more times in their lives.
There are myriads of ways for the lumbar roots and sciatic nerve to get irritated, including, but not limited to: a nerve pinch, disk herniations, and genetic abnormalities. However, what’s important to remember, is that generally, nerve impingement doesn’t cause pain, inflammation does. In fact, the majority of the time, Sciatica is referred pain from the lower back and doesn’t even result from nerve-root compression. How one person reacts to load, movement, or even stretch, can be very different across the spectrum of people, and it’s likely that some people have nerve roots that are just a little quicker to react. Those with Fibromyalgia suffer from abnormalities in the way that the brain deals with pain. Supraspinal processes have a top-down enhancing effect on nociceptive processing in the brain and spinal cord. Studies have begun to suggest that such influences occur in conditions such as fibromyalgia. This means that those who do have Fibromyalgia and sciatica, they may be far more sensitive to noxious stimuli compared to the general population. Factoring in changes in tissues, stress, load, and movement, and those with Fibromyalgia may be more prone to reacting to these changes byways of producing pain.
Very rarely is sciatica mechanical in nature. Even issues like nerve impingement are fairly difficult to occur, due to the abundance of room at the nerve root. There are also many cases of actual impingement, where the individual doesn’t even have any pain.
I’m not writing to scare you, as the wide majority of cases of sciatica are completely harmless. However, it is important for you to understand that self-diagnosing sciatica is not a good idea. If it is troublesome, comes with a wide range of completely new symptoms, or you are worried, consult your doctor and get checked out. Whilst you very well could have Sciatica, there are a few other things that can often mimic sciatica, things such as;
- Piriformis syndrome
- Genic abnormalities, wherein the sciatic nerve actually runs through the piriformis muscle, instead of under it.
- Joint problems in the spine
- Sacroiliac joint dysfunction
- Cauda Equina syndrome
- And less likely, things like cluneal nerve entrapment.
Generally, red flags when it comes to sciatica are;
- Bowel/bladder dysfunction
- Progressive neurological weakness.
- Saddle anaesthesia.
- Incapacitating pain.
- Unrelenting night pain.
- Sexual dysfunction
- A cold feeling in the feet or toes
- An itchy feeling in the painful regions of the leg that provokes the urge to scratch (pruritus)
This article covers:
ToggleWhat to do?
Keep relatively active
Bed rest has been a popular treatment for sciatica and back pain for the better part of the last few decades. In terms of published evidence, most meta-analyses and reviews show that there are no significant benefits to bed rest over staying active when it comes to sciatica pain (and vice versa). However, as mentioned in a review posted in Spine, there is no considerable difference between advice to stay active and advice for bed rest, and there are potentially harmful effects of prolonged bed rest, it is reasonable to advise people with acute low back pain and sciatica to stay active.
So, if you do have fibromyalgia and sciatica, you have been checked out and there are no red flags, keeping active can be very helpful. However, being active doesn’t mean you need to be doing crazy exercises, it just means getting up and moving around, as much as the pain will allow.
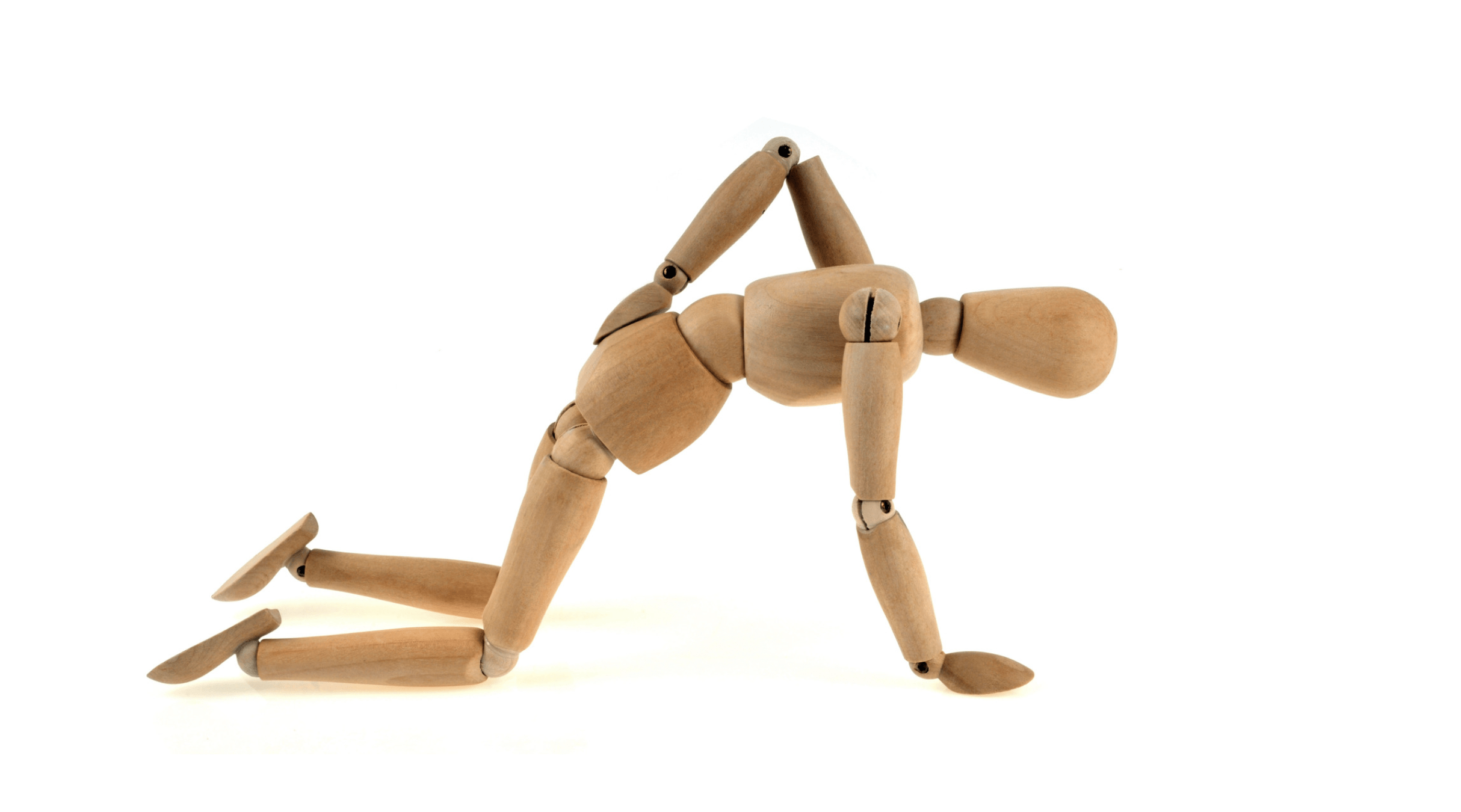
In terms of movements, gentle dynamic movement that helps to move a joint through its full range can be incredibly beneficial when it comes to sciatica, helping us to utilise our own internal pain killers. Likewise, stretching can be incredibly beneficial, helping to calm the nervous system down, reduce muscle tone and guarding, reduce pain, and to help create a sense of safety. This sense of safety is a particularly interesting topic, as fear will cause you to guard, making you stiffer and most likely in more pain.
Heat and Vibration
Heat can also be used on the surrounding muscles to help them relax. Due to the thickness of the tissue in the buttocks, heat isn’t going to have much of a circulatory effect on the nerves or muscles that can irritate sciatica. However, it will provide enough input to help calm down the nervous system. A good heat pad or warm bath is sufficient.
Likewise, vibration can be used for sciatica with a fairly good outcome. Vibration therapy may help to reduce muscle soreness and interleukin-6, helping to stimulate lymphocyte and neutrophil responses, a useful modality in treating muscle inflammation. Which, if we learned anything today, is most likely more important than impingement.
– Adam –
Enjoyed Our Blog? Why Stop Here?
If you’ve found value in our posts, imagine the impact of a structured, science-backed course tailored specifically for fibromyalgia and its unique challenges. The Full Body Fibro Course is your ultimate starting point for understanding your body, improving mobility, and managing symptoms effectively.
FAQ on sciatica
Yes, it is possible to have both fibromyalgia and sciatica simultaneously. Fibromyalgia is a chronic condition characterised by widespread pain and sensitivity, while sciatica is a specific type of pain caused by irritation or compression of the sciatic nerve. The presence of fibromyalgia can make the pain from sciatica feel more intense due to sensitisation.
It is generally not advisable to push through severe sciatic pain, as this can worsen the condition. Instead, focus on gentle activities and movements that do not exacerbate the pain.
Yes, in severe cases, sciatica can be so painful that it impairs your ability to walk. If you experience debilitating pain, numbness, or weakness in your legs, it is crucial to seek immediate medical attention to prevent further complications and receive appropriate treatment.
Walking can help alleviate sciatica symptoms by promoting circulation and reducing inflammation. However, walking at a comfortable pace and avoiding overexertion is important. Consult a healthcare professional for guidance on appropriate exercises and activities to manage sciatica pain effectively.
The four stages of sciatica can be described as acute, subacute, chronic, and resolution:
Stage 1: Acute Sciatica
Acute sciatica is the initial and most common form, typically resulting from a herniated disc or spinal stenosis compressing or irritating the sciatic nerve. Symptoms often include sharp pain, tingling, numbness, and lower back or leg weakness.
Stage 2: Subacute Sciatica
Subacute sciatica is marked by mild to moderate pain that persists for several weeks. During this stage, individuals may experience intermittent pain and muscle spasms, which can fluctuate in intensity.
Stage 3: Chronic Sciatica
Chronic sciatica refers to pain that lasts for more than six weeks. The symptoms can vary widely, ranging from mild discomfort to severe pain, and may include muscle weakness, numbness, or a burning sensation in the affected areas.
Stage 4: Resolution
Resolution is the final stage, where the symptoms of sciatica significantly decrease or completely disappear. This stage indicates that the underlying cause of sciatica has been addressed, allowing the individual to resume normal activities without pain.
There is no instant cure for sciatica, but several treatments can help alleviate the pain quickly. These include physical therapy, stretching exercises, anti-inflammatory medications, heat therapy, and in some cases, corticosteroid injections. Consult a healthcare professional to determine the most effective treatment for your condition.