- POTS and Exercise: The First Step Everyone Misses - 27 June 2025
- The Missing Link Between Breathlessness, Fatigue, and Chronic Pain: Understanding CO₂ Tolerance - 19 June 2025
- What is Mast Cell Activation Syndrome? - 12 May 2025
Greetings from our corner of the web! Have you ever heard of Ehlers-Danlos syndrome (EDS)? Or perhaps you, or someone close to you, have been noticing symptoms like joint hypermobility, unusually stretchy or fragile skin, or perhaps bruises appearing at the slightest touch? If so, you’re in the right place. EDS represents a collection of rare inherited conditions that primarily target the connective tissue – the unsung hero that lends support to various parts of our body, be it the skin, joints, or even our vital organs. Dive into this article as we unravel the mysteries of EDS, shedding light on its various types, the tell-tale symptoms, the intricacies of diagnosis, and the myriad of treatment avenues available.
Decoding Ehlers-Danlos Syndromes
Ehlers-Danlos syndrome (EDS) isn’t just a singular condition; it’s a multifaceted enigma that manifests differently in each individual. At its core, EDS arises due to glitches in specific genes responsible for connective tissue integrity. Imagine the connective tissue as the body’s scaffolding; any weakness can lead to a cascade of symptoms. While some might face only mild inconveniences, others might grapple with debilitating manifestations. The origins of EDS can be traced back to our genetic code – it can be an inheritance from one or both parents or sometimes, nature throws a curveball in the form of a spontaneous genetic mutation.
Now, EDS isn’t a one-size-fits-all label. There are thirteen distinct types, each with its signature symptoms and characteristics. The most prevalent among these is hypermobile EDS (hEDS). Picture this: joints that move beyond the usual range, akin to a contortionist, accompanied by joint pain, skin that bruises as if it were peach, and a host of other symptoms. But that’s just the tip of the iceberg. The EDS spectrum also includes classical EDS (cEDS), vascular EDS (vEDS), and kyphoscoliotic EDS (kEDS), each presenting its unique challenges.
Navigating the maze of EDS diagnosis can be daunting. With the absence of specific tests for most types, diagnosis hinges on a thorough medical history, a keen physical examination, and ticking off specific clinical criteria. Occasionally, genetic testing might step in to solidify the diagnosis. If EDS is a suspect in your health puzzle, it’s paramount to seek a seasoned healthcare professional well-versed in the nuances of EDS. Their expertise can be the beacon guiding you towards an accurate diagnosis and a tailored management strategy.
Hypermobile EDS (hEDS): This is one of the most prevalent types of EDS. Individuals with hEDS often exhibit joint hypermobility, which means their joints can move beyond the normal range. Picture a gymnast’s flexibility, but with potential repercussions like joint pain, frequent dislocations or subluxations, and that unsettling sound of clicking joints. But it doesn’t stop there. Fatigue, easy bruising, digestive issues, dizziness, and even bladder control problems can be part of the package. Sounds challenging, doesn’t it? But remember, with the right care and management, these symptoms can be mitigated.
Classical EDS (cEDS): This variant tends to have a more pronounced effect on the skin. Those with cEDS might find their skin to be stretchy and fragile, reminiscent of the delicate pages of an old book. Minor accidents can lead to skin tearing or extensive bruising. Wounds might take their sweet time to heal, often leaving behind scars that are wider than usual. And if that wasn’t enough, they might also face challenges like hernias and organ prolapse.
Vascular EDS (vEDS): Now, this is a more severe and rare type of EDS. It primarily affects the blood vessels and internal organs. Imagine skin so thin that the blood vessels are visible, almost like a roadmap of life. This fragility also extends to the blood vessels themselves, which can rupture, leading to life-threatening internal bleeding. The risks also encompass potential organ issues, such as tearing of the bowel or womb. Other signs might include hypermobile fingers and toes, distinct facial features, and varicose veins.
Kyphoscoliotic EDS (kEDS): Another rare variant, kEDS is characterized by a curvature of the spine, joint hypermobility, muscle tone that’s weaker than usual, fragile eyes, and skin that’s both soft and stretchy. Bruising easily and scarring are also common symptoms.
Diagnosis of EDS can indeed be a bit of a puzzle. There’s no one-size-fits-all test to pinpoint the condition. Instead, it’s a combination of delving into one’s medical history and a thorough physical examination. In certain scenarios, genetic testing might be the key to unlocking the mystery, especially for specific EDS types. If you suspect you might have EDS, it’s crucial to consult with a healthcare professional, perhaps a rheumatologist or geneticist, who’s well-versed in the nuances of EDS.
While we might not have a magic wand to wave away EDS, many of its symptoms can be managed with the right support and treatment. This could involve a team of healthcare professionals, from physiotherapists to occupational therapists and even counsellors. Their combined expertise can help devise strategies to bolster joints, alleviate pain, enhance daily activities, and tackle any emotional or psychological hurdles.
Living with EDS is akin to walking a tightrope. One must exercise caution, especially with activities that might strain the joints or heighten injury risk. Yet, it’s equally essential not to cocoon oneself and miss out on the joys of life. Depending on the EDS type and its severity, recommendations might range from low-impact exercises like swimming or pilates to techniques for conserving energy and pacing oneself.
The way EDS is passed down through generations can vary. Some types follow an autosomal dominant pattern, where a single faulty gene from one parent can lead to a 50% chance of their offspring developing the condition. Others might follow an autosomal recessive pattern, where both parents pass on the faulty gene, leading to a 25% chance for their children. Genetic counselling can shed light on these patterns and their implications for future generations.
Diagnosis of Ehlers-Danlos Syndromes (EDS)
Ehlers-Danlos Syndromes (EDS) are a group of connective tissue disorders that can be inherited. They are generally characterized by joint hypermobility (joints that stretch further than normal), skin hyperextensibility (skin that can be stretched further than normal), and tissue fragility. The diagnosis of EDS is based on a combination of clinical criteria, physical examination, and in some cases, molecular testing.
Types of EDS and Their Diagnostic Criteria:
- Spondylodysplastic EDS (spEDS):
- Major criteria: Short stature (progressive in childhood), muscle hypotonia (ranging from severe congenital to mild later-onset), and bowing of limbs.
- Diagnosis: Requires the first and second major criteria, characteristic radiographic abnormalities, and at least three minor criteria (either general or gene-specific). Molecular testing is essential for a final diagnosis.
- Musculocontractural EDS (mcEDS):
- Major criteria: Congenital multiple contractures, characteristic craniofacial features evident at birth or early infancy, and characteristic cutaneous features.
- Diagnosis: In early childhood, major criteria 1 and 2 are required. In adolescence and adulthood, major criteria 1 and 3 are necessary. Molecular testing confirms the diagnosis.
- Myopathic EDS (mEDS):
- Major criteria: Congenital muscle hypotonia, proximal joint contractures, and hypermobility of distal joints.
- Diagnosis: The first major criterion plus either another major criterion or three minor criteria. Molecular testing is essential for a final diagnosis.
- Periodontal EDS (pEDS):
- Major criteria: Severe and intractable periodontitis of early onset, lack of attached gingiva, pretibial plaques, and a family history of a first-degree relative meeting clinical criteria.
- Diagnosis: The first or second criterion, plus at least two other major criteria and one minor criterion. Molecular testing confirms the diagnosis.
- Arthrochalasia EDS (aEDS):
- Major criteria: Congenital bilateral hip dislocation, severe general joint hypermobility, and skin hyperextensibility.
- Diagnosis: Requires congenital bilateral hip dislocation plus either skin hyperextensibility or severe general joint hypermobility with at least two minor criteria. Molecular testing is essential for a final diagnosis.
- Dermatosparaxis EDS (dEDS):
- Major criteria: Extreme skin fragility and characteristic craniofacial features.
- Diagnosis: Requires the two major criteria plus either another major criterion or three minor criteria. Molecular testing confirms the diagnosis.
- Kyphoscoliotic EDS (kEDS):
- Major criteria: Congenital muscle hypotonia, congenital or early onset kyphoscoliosis, and general joint hypermobility with dislocations/subluxations.
- Diagnosis: Requires the first two major criteria plus either the third major criterion or three minor criteria. Molecular testing is essential for a final diagnosis.
Each EDS type has a set of clinical criteria that help guide diagnosis. A patient’s physical signs and symptoms are matched up to the major and minor criteria to identify the type that is the most complete fit. Molecular diagnostic strategies, such as Next-Generation Sequencing (NGS) technologies, offer the potential for parallel sequencing of multiple genes, making the diagnosis more accurate.
In the intricate journey of understanding and diagnosing Ehlers-Danlos Syndrome (EDS), it’s paramount to recognise the multifaceted nature of this condition. From clinical evaluations to genetic testing, the diagnostic process is a blend of meticulous observation and advanced medical techniques. As we’ve delved into the depths of EDS, it’s evident that a holistic approach, considering both physical manifestations and underlying genetic factors, is crucial.
The journey might be complex, but with the right knowledge and resources, like the insights shared in this document, one can navigate the path to diagnosis with clarity and confidence. Remember, understanding is the first step to managing and living harmoniously with EDS.
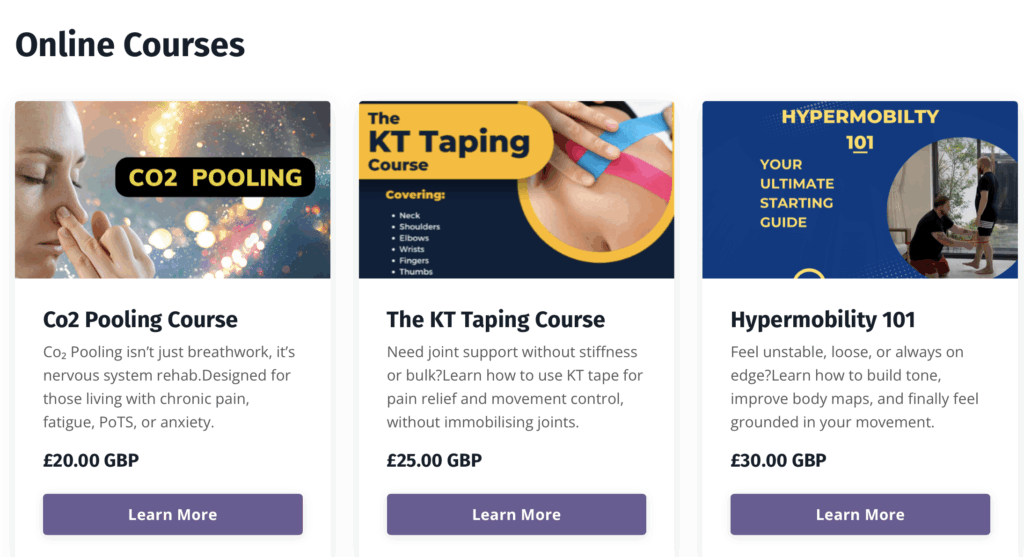
Enjoyed Our Blog? Why Stop Here?
If you’ve found value in our posts, imagine what you’ll gain from a structured, science-backed course designed just for you. Hypermobility 101 is your ultimate starting point for building strength, stability, and confidence in your body.