- POTS and Salt: What the Science Actually Says - 18 February 2026
- Why the Beighton Score Matters More Than It Should - 18 February 2026
- Brain Fog in EDS, POTS and Long COVID: Causes and Practical Ways to Cope - 13 February 2026
It’s not uncommon for those with Hypermobility and EDS to have difficulty with sleep, sleeping positions, getting to sleep, and last but not least, staying asleep. Subluxating/dislocating joints, gastric issues, pain, and even anxiety are all factors that many of those with conditions like Ehlers-Danlos syndrome and hypermobility struggle with when it comes to sleeping.
With so many with hypermobility struggling with sleep, you would expect to find more information on sleeping better. However, when looking online, you find the same old advice, tips and tricks across the internet. Relax before bed, and don’t use screens. Blah, blah, blah.
So, the purpose of writing this article is to give those with hypermobility who struggle with sleep good, targeted advice that’s not the same old stuff you find littered across the internet. However, I am going to go deep. Hypermobility complicates sleep massively, and if we want to improve our sleep when hypermobility is concerned, we have to cover many areas. This way, we become armed with the information we need to give ourselves the gift of good sleep.
This is a beast of an article, with a lot of information and the sole aim of teaching you what you need to know and looking at the complications to sleep that hypermobility often causes.
So, if you’re ready to improve your sleep, let’s go!
This article covers:
ToggleLack of sleep increases pain
The relationship between sleep disturbances and pain has been widely studied (1). Largely showing us that with sleep disturbances comes an increase in pain. It is not only well established that poor sleep directly causes more pain, but also a sharp decline in physical functioning and mood, especially during the early parts of the next day (2). Similarly, studies show that a good night’s sleep only appears to offer a temporary respite to pain, nudging us further down the rabbit hole that pain is an incredibly complex beast and often, at times, just plain weird. Additionally, lack of sleep can be one of the main contributing drivers of EDS flare-ups, often manifesting as increased pain and fatigue.
Interestingly, and contrary to popular belief, you can not bank sleep. Chronic sleep deprivation or a few bad nights can’t be remedied by one long sleep at the weekend. At least, that is what the evidence suggests.
Several large prospective studies suggest that prolonged sleep problems may even increase the risk of developing chronic pain in the future for healthy individuals (3). So, right from the outset, we can see just how important sleep is for the general population. But does being hypermobile affect sleep? And if it does, to what degree?
We mention briefly the impact of not getting enough sleep, but on the other side of the coin is that consistently good sleep has a remarkable and extremely profound effect on mood, cognitive functions, and health in general. Furthermore, and most importantly for you reading this article, if you are hypermobile, good sleep moderates the relationship between pain interference, depression, and hypermobile anxiety, in those with chronic pains much so, such that good sleep quality reduces the effect of pain interference when it comes to depression and pain.
Whilst many people with Hypermobility and EDS search for areas of their lives to focus on to better their health, sleep is, unfortunately, one of the more difficult areas to address. Recurrent subluxation/dislocations during sleep, the feeling of “tired but wired,” and pain, in general, all factor into creating these sleep disturbances that often increase pain and decrease mood.
One small survey of EDS patients in 2001 showed increased difficulties with sleep in the population. It was estimated that of those with EDS, 56% had difficulty maintaining sleep (4). So you are not alone; sleep problems have become almost a staple when it comes to Ehlers-Danlos syndrome and hypermobility.
I imagine you clicked on this article with one intention: to find out how to get better sleep when you have hypermobility.
So, this article is about sleep. It is a deep dive into how hypermobility affects it and what you can do at home to help you get better, more rested sleep.
Why do we even need sleep?
Sleep as a whole is an incredibly important function, however, we still are not entirely sure why we sleep in the first place No, seriously, we have theories that cover restorative reasons for sleep, all the way to brain plasticity theories. But we still don’t have a definite answer as to why we need to sleep.
However, we do know that sleep is essential for us. Among other things, sleep helps our cerebrospinal fluid effectively wash our brains, eliminating accumulated metabolic waste and memory-impairing proteins (5). It keeps our immune system healthy, as lack of sleep impairs our bodies’ innate ability to release infection-fighting antibodies, as cells are reduced during periods when you don’t get enough sleep. And probably most known to all, sleep helps us to release growth hormones and repair tissue.
Unfortunately, humans don’t possess any neat tricks when it comes to sleep, like, say, the dolphin, which can pretty much switch one side of its brain off to sleep while using the other side to stay alive and function. With the average human sleeping for around 25 years of their life, we need to ensure that we get enough sleep because if we don’t, the problems that can occur are numerous.
For those with EDS or Hypermobility Syndrome who don’t get enough sleep, the same issues are present that occur in the general population, but also other issues can occur. Most prominently, there is a major link between tissue repair and sufficient sleep. The proper time for the body to repair and rebuild tissue is particularly important for those with tissue connectivity problems: it is sorely needed to heal from dislocations. With joint dislocations being fairly common with hypermobility, we must sleep to heal any damage sustained.
Sleep complications for those with Hypermobility and EDS
As we previously mentioned, sleep is important for repair, especially when healing joint sprains, subluxations, and injuries. However, many other issues can present themselves when you are hypermobile, which the general population is not privy to.
Increased risk of joint subluxation/dislocation
When we are in too much pain to sleep or if we have difficulties getting into a comfortable sleeping position, it can often leave those with hypermobility to be laid wide awake for hours. Unfortunately, with a lack of sleep also comes a decline in cognitive function (6). This decline can be especially detrimental for those with hypermobility, as not being present and aware due to tiredness can create the perfect environment for subluxation/dislocations to occur. After all, dislocations and subluxations increase when unaware of our environment. If you are too tired to focus when walking, it’s fairly easy to misjudge a step or a curb and sublux an ankle joint. Or perhaps more closer to home for those of you reading, you bend over to grab something and are hit with a rib subluxation.
Gastric Issues
Another issue that interferes with creating a good sleeping pattern for those with Hypermobility/EDS is gastric issues. Proinflammatory cytokines, such as interleukin-1 and interleukin-6, have been strongly associated with sleep dysfunction (7). These cytokines have been altered in certain gastrointestinal diseases, such as gastroesophageal reflux and inflammatory bowel disease. With a strong body of evidence that supports changes in cytokine release and specificity in gastrointestinal disorders affecting the sleep-wake cycle. One thing seems certain: gastric issues are likely to affect sleep, and poor sleep is likely to affect gastric issues, often compounding issues, leasing to problems with EDS and nutrition.
Numerous studies have shown that patients with IBS and/or functional dyspepsia also report poor sleep. A survey of 2936 patients found that the presence of functional dyspepsia and IBS was a statistically significant risk factor for poor sleep (8). If you’re hypermobile, it’s very important to understand your hypermobility dietary needs. The right nutrition can help manage heds symptoms more effectively, support joint health, reduce inflammation, and improve your sleep, which, as we know, is very important.
Whilst gastric issues can cause poor sleep, a few studies also show that chronic sleep deprivation can exacerbate issues like colonic inflammation. So, unfortunately, it’s a somewhat chicken-and-egg situation.
GERD
GERD is another common problem affecting sleep in those with hypermobility. Gastroesophageal reflux disease (GERD) occurs when stomach acid repeatedly flows back into the tube connecting your mouth and stomach (oesophagus). This backwash (acid reflux) can irritate the lining of your oesophagus. GERD has been well documented in those with hypermobility and EDS, often prevalent in upwards of 50% of the population in some studies (8). I can personally attest to this one, which is one of the reasons why I no longer eat late at night: It’s just not worth it.
Interestingly, a population study of over 6500 patients in Norway found that the risk of GERD symptoms in patients with insomnia was 3 times greater than in those with no sleep complaints. These studies suggest that most people with GERD have astounding night-time symptoms, which result in an increased risk of sleep disturbances.
Vitamin D deficiency
Deficiency in Vitamin D is common in those with hypermobility aEhlers-Danloslos syndrome and has often been attributed to poor sleep. However, the evidence between vitamin D deficiency and poor sleep is somewhat controversial. Some studies suggest a link between them, however, much more research of higher quality and with bigger cohorts, needs to be done.
The general thinking is that vitamin D receptors and the enzymes that control their activation are expressed in several brain areas that are involved in sleep regulation. Vitamin D is also involved in the pathways that help produce Melatonin, the hormone involved in regulating your sleep and wake cycle. So, it does look like Vitamin D may have either a direct or indirect role in regulating sleep. While vitamin D deficiency has been associated with sleep disorders, the evidence is still a little thin to concretely support the role of vitamin D supplementation in preventing or treating sleep disturbances.
Let it be known that even if it doesn’t help sleep, there are still numerous other reasons to get checked for low Vitamin D.
Obstructive Sleep Apnoea
There is also another fairly common problem that can affect the sleep of those with hypermobility: Obstructive Sleep Apnoea(OSA)
Obstructive sleep apnea (OSA) is a relatively common condition in which the walls of the throat relax and narrow during sleep, interrupting normal breathing. This may lead to regularly interrupted sleep, which can have a big impact on quality of life and increase the risk of developing certain conditions.
Obstructive sleep apnea was once very underestimated in those with hypermobility and EDS (9); however, with more research and funding going into this area, it’s starting to show that it might not be all that uncommon. Whilst more research does need to be done to identify the prevalence amongst the different subtypes of EDS, it’s a definite move forward.

With connective tissue disorder comes, well, disorders with the connective tissue. As your nose, throat, and maxilla (upper jaw) all consist of connective tissue, they can be affected by EDS and hypermobility. Upper airway instability and recurrent, partial or complete blockages have the potential to cause sleep apnea. This can lead to drops in oxygen levels, sleep disturbances, and unrestful sleep.
Some studies even found the prevalence of OSA in EDS to be around 30% (10). This is important to note, as OBE is notorious for causing excessive daytime sleepiness and impaired quality of life.
If you do believe you may have OSA, then your first port of call should be to visit your doctor to express your concerns. OSA is fairly easy to diagnose, and treatment can yield immediate relief.
If EDS has caused you to struggle with sleep apnea, consider talking to your doctor about different sleeping positions and a Continuous Positive Airway Pressure (CPAP) machine that will help keep your breathing regular throughout the night and bring about a more restful sleeping experience.
The Autonomic Nervous System
To further understand the relationship between sleep disturbances and hypermobility disorders, we must consider the role of the Autonomic Nervous System. A normally functioning ANS continuously “fine-tunes” body systems in response to both internal and external stimuli to maintain homeostasis. When not functioning properly, which is common in people with hypermobility disorders, the ANS is unable to keep the body in a steady state, further contributing to fatigue and decreased quality of life by affecting the natural sleep cycle.
Likewise, I want to draw your attention to something that gets missed a lot of the time: Thoracic outlet syndrome(TOS)
We have noticed that the vast majority of our hypermobile clients with severe dysautonomia have, to some degree, Thoracic outlet syndrome.
TOS is prevalent in a lot of those with Postural Orthostatic Tachycardia Syndrome (POTS), another dysautonomia condition commonly associated with Ehlers-Danloslos syndrome.
Thoracic outlet syndrome (TOS) is a constellation of symptoms resulting from neurovascular compression at the thoracic outlet, causing some combination of pain in the neck and upper extremities, weakness, sensory loss, paresthesia, swelling, and even discolouration. What classification of TOS you receive depends on the anatomical structure that is being compressed: venous compression of the Subclavian vein, arterial compression of the subclavian artery, and neurogenic compression of the brachial plexus.
It’s not a mad assumption to think that compression of vascular and Neurogenic structures will cause sleep issues. Pins and needles, radiating pain, and weakness are all contenders for affecting sleep. Likewise, compression of sympathetic fibres forming the cardiac plexus may increase cardiac sympathetic activity and result in nighttime heart palpitations.
If you do have TOS, it is important to avoid sleeping positions that increase the pressure on the outlet. Generally, we recommend sleeping on your back or with two pillows on the affected side to prevent outlet compression. Likewise, KT tape may be a good idea!
Whilst KT tape gets a lot of praise, when in fact it likely doesn’t do anything of what it claims), some studies do show that it can provide benefits in terms of relieving pain and paresthesia and improving upper limb function and quality of life in those with TOS. So that’s something.
Bruising and sore spots
Due to the increased fragility of dermal blood capillaries and poor structural integrity of the skin, easy bruising is often seen as a hallmark of many subsets of Ehlers-Danloslos syndrome, including the hypermobility type.
Certain sleeping positions may cause you to bruise or develop sore spots if your mattress is too hard. Yet, too soft a mattress can lead to uncomfortable sleeping positions and stiffness the next day. There are many “chicken and the egg” scenarios with hypermobility and sleep; unfortunately, this is yet another one. So, with all of the above in mind, let’s take a look at the different things to consider when trying to sleep with hypermobility and Ehlers-Danlos syndrome.
Sleep positions for those with Hypermobility and EDS
One of the first things we should look at is sleep positions. If you’re going to be lying in bed for 8 hours, you need to be in a comfortable position and a position that isn’t going to cause issues. Depending on you as an individual, with individual joints and specific issues affected by hypermobility, you will need a sleep position that works best for you and your issues (a video on this later to help you).
Some people may find that sleeping on their left side helps with gastric issues and allows for a night of better sleep, but this may be the worst position to sleep in for someone with recurring shoulder subluxations.
Whilst the side sleeping position seems to be the most popular for the general population, what do those with EDS and hypermobility find as the most comfortable positions? Now, there wasn’t a lot of data on this to look at. So, without real data, we asked our hypermobile and EDS followers on our Facebook and Instagram pages.
The results
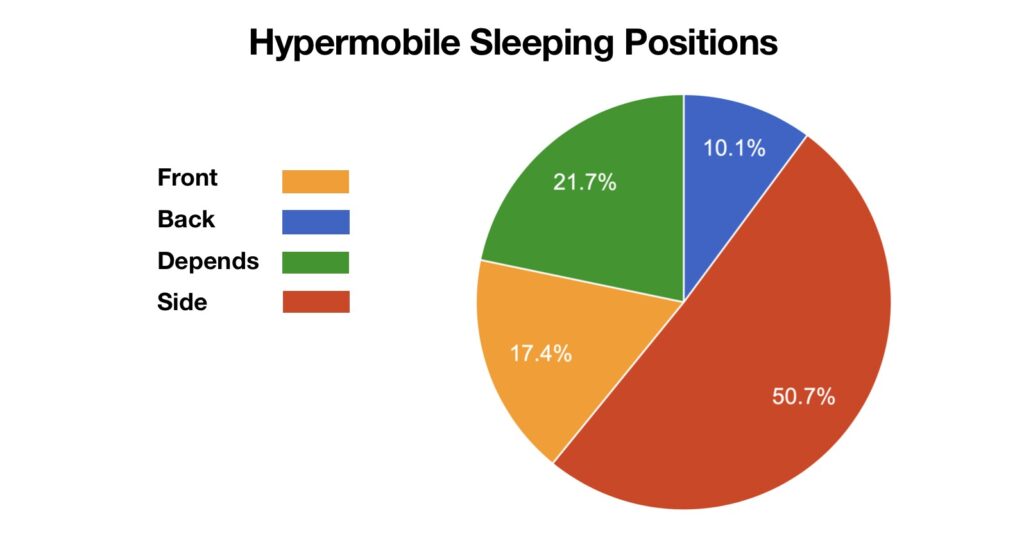
Remember that this isn’t a strict scientific experiment or done with thousands of people. However, we have a fairly large following on social media, so we did have a decent data set to look at. But, the kind of people who follow us, and many other factors may skew data, it is just how it goes.
We found that:
50.7% Preferred side position sleeping.
10.1% Preferred sleeping on their back.
21.7% Changed their position depending on pain at the time.
17.4% Preferred sleeping on their front.
The results show a clear preference for side sleeping in those with hypermobility and EDS, or at least those who follow us on social media and participated in this little experiment. Much like the general population, those with hypermobility also prefer sleeping on their side. Additionally, from our survey we found that endometriosis in EDS was also a huge factor affecting sleep.
As we start to explore what we can do to help with sleep, let us first explore some of the pros and cons of each sleeping position when it relates to hypermobility. Why may they help you, but also what problems they may cause?
Sleeping on your front

Favoured by 17% of those with EDS and hypermobility in our little experiment, sleeping on your stomach isn’t very popular amongst those with connective tissue disorders. Sleeping on your front requires you to turn your head to one side, at least if you want to continue breathing. Holding body parts in prolonged positions is uncomfortable, regardless of the body part. We have an inbuilt system that tells us when it’s time to change our position and posture; it’s called discomfort, and it works well.
Staying in one position for too long activates high threshold nerves(nociceptors) that detect things that might be potentially bad for us: too much pressure, stretch, load, etc. These nerves allow us to avoid getting hurt or damaged by actual or potential threats. Staying in one position for too long changes the blood flow, nerve sensitivity, and tissue tone. Ultimately, this forces our brain to either say, “Hey buddy, I think it’s time to move”, or, in some cases “, Wow, wow, this is dangerous, untolled danger; here, have some pain, so you remember not to do this ever again!” Brains can’t live with them; can’t live without them.
Likewise, sleeping on your front with your head turned to one side isn’t just going to cause sleep disturbances. It’s likely going to cause some modulation of your nervous system. Holding a muscle in a lengthened and weaker position for several hours may illicit certain protective measures being initiated by your brain, namely, causing your neck to become more painful and far more sensitive. Oh, and probably headaches as well.
There are also issues with the ribs. Many with hypermobile and EDS are prone to rib subluxations. Putting direct pressure through the ribs and the lower, less stable floating ribs may cause pain and even subluxations during the night, definitely causing sleep disturbances.
However, some people with hypermobility seem to like this position, so there must be a few pros, right?
Well, sleeping on your front can sometimes help digestion, which is good for those with gastric issues. But possibly one of the only real reasons to sleep on your front is that it can help relieve breathing difficulties caused by sleep apnea, which, if we remember from the paragraphs above, is pretty common in EDS and hypermobility.
Sleeping on your side

In our little experiment, side sleeping was favoured by 50% of those with EDS and hypermobility. With so many people choosing their sleeping position, let us explore why.
Side sleeping, especially on the left side, has been shown to reduce symptoms of Gastroesophageal reflux disease (GERD) (11). Whilst the exact mechanisms are still not agreed upon, it’s most likely limiting the amount of stomach acid exposed to the oesophagus due to gastric fluids sitting at a lower level than the oesophagus when laying on your left side.
So, sleeping on your left side can help with digestion and common gastric issues such as GERD, but what about the right side?
Interestingly, right-slide sleeping is the position that those with heart issues tend to naturally favour during sleep. Likewise, perhaps a pro for side sleeping on the right is that it helps to avoid heart palpitations. Laying on your left side may stimulate the vagus nerve, sending abnormal electrical signals to the heart and causing palpitations. It’s nothing to worry about, but it’s likely to scare you and disrupt your sleep.
We mentioned earlier that sleep helps our cerebrospinal fluid effectively wash our brains, eliminating accumulated metabolic waste and memory-impairing proteins. Well, emerging studies show that side sleeping may be the optimal position for this to occur (12). So, that’s a pretty big win for side sleepers.
Another reason people find side sleeping so alluring is that, like front sleeping, it helps reduce snoring. Now, this may not be your favourite sleeping position, but it may be a sleeping position that your partner prefers for you. My wife has often given me a loving but pretty dam firm elbow to the ribs mid-sleep. Reminding me to roll onto my side and to stop snoring. In my case, if I sleep on my side, it avoids the many preventable sleep disturbances that my wife will cause me if I disturb her sleep with my snoring.
Another win is that side sleeping when hypermobile appears beneficial for Sleep apnea, another common condition amongst those with hypermobility (13). This makes sense as side sleeping expands the upper airway lumen, especially the retroglossal space.
But, with every pro comes the potential for a con; such is usually the case with hypermobility!
Whilst so many hypermobile and EDS people seem to prefer the side sleeping position, there are, as with anything, those who do not. Side sleeping can be notorious for hypermobile joints, especially the shoulders, hips, and SI Joints. Prolonged periods with the hip stacked on top of the hip can often result in pain and soreness. Likewise, as we drift further into sleep, it is fairly easy for one leg to move forward of the other one, effectively leaving the hips twisted for several hours. As the nociceptors (danger nerves) of those with hypermobility appear more sensitive than the general population, this opens a pretty big can of worms. Most likely, creating issues with joint pain and stability issues at the hips and SI Joints.
There are also issues with the shoulder that can occur with side sleeping. We mentioned previously issues like Thoracic Outlet Syndrome (TOS), and this is something that can be made worse when side sleeping. Tingling/numb fingers, pins and needles, and a reduction in blood flow will all cause you to wake up due to discomfort or a racing heart. Likewise, side sleeping can have the potential to cause shoulder subluxations/dislocations for those with hypermobility. A great way to help manage and mitigate these issues is with some good sound rehab exercises; you can find some in our hypermobility rehab resources section on the website.
Sleeping on your back

Favoured by only 10% of those with EDS and hypermobility in our little experiment, sleeping on the back seems to be the least popular position amongst those with EDS and hypermobility. To be honest, this doesn’t come as a surprise. Back sleeping is directly linked to making issues like sleep apnea worse, causing restrictions of air and causing multiple sleep disturbances. When we consider how many of those with hypermobility have sleep apnea, back sleeping doesn’t seem like a good idea.
Back sleeping is also linked to (although not understood why) sleep paralysis, with episodes more frequently associated with those who sleep on their back. Perhaps it has nothing to do with the sleep position at all, but more so that people who experience it are more likely to choose back sleeping. But, I thought I would mention this as I do love a weird fact!
Sleeping on your back also locks your spine into one singular position, and as you will remember from earlier, bodies don’t like to be restricted when it comes to movement.
It’s not all doom and gloom, though, as back sleeping can do one thing that a lot of other positions simply cannot: evenly distribute weight. Sleeping on your back allows your body weight to be evenly distributed across the widest surface of your body, minimizing pressure on body parts and keeping hypermobile joints in alignment. This position single-handedly gives those with hypermobility the best joint positions during sleep, especially if many pillows around the body are used.
However, back sleeping may cause lower back pain and increase the risk of issues with acid reflux, so it’s another trade-off for hypermobility. Looking at the above, it’s no wonder why it’s the least favoured position for those with hypermobility and EDS.
Changing sleeping positions
Our second favourite sleeping position for those with EDS and hypermobility, at a whopping 20%, was changing sleeping positions depending on the pain at that time or during the night. This makes a lot of sense as to why it is so popular. After all, if your shoulder was fine last week when you were sleeping, but dislocated ed this week, then back sleeping is going to be better for the shoulder. But, we still hit the problems of different comorbidities that come with EDS and hypermobility. Issues like GERD and sleep apnea. Whilst a normal side sleeper may switch to back sleeping because of hip pain, issues like sleep apnea and Gerd have the potential to cause even more sleep disturbances. Often more than what the shoulder would have caused.
What can often occur for this subset of EDS and hypermobility sleepers is that they end up playing a night-time game of “chase the pain”. They lay on their back for a little while until their back hurts or reflux kicks in. Then they turn over to their side to let their reflux settle down, and their back pain lessens, only for their shoulders to start hurting, forcing them into another position. Effectively, they spend the entire night trying to outrun various issues and pain.
Finding your sleep position when hypermobile
So, we looked at the sleeping positions that those with hypermobility often choose. What you have probably noticed by now is that with hypermobility and sleeping positions, it is the other issues that come with hypermobility that cause most of the problems with sleeping. A generic, do this or sleep in this exact way is not going to help you. You must determine which sleeping position is best for you and your joint, gastric, or breathing issues.
But don’t worry, you’re not alone in this. I have worked with and helped hundreds of people with hypermobility and EDS, tweaking and modifying sleeping positions so that they work for them and their issues. Each sleeping position has many modifications you can make so that it helps your main issues without causing multiple others. Now, this gets complicated, and text isn’t good for visual teaching, so let’s cover the next section via video.
Sleep set up for those with hypermobility
So, we covered sleeping positions, but did you know that the width of your hips and the firmness of your mattress are two key contenders in you wake up stiff and aching? This is why we need to cover your sleep setup. Your sleep setup is just as important as your sleeping position. Your sleep set-up refers to the items that form part of your sleeping routine: sleeping masks, mattresses, pillows, etc.
Mattress
A good mattress is one of the best investments for sleep health; find one that is firm but not too hard so that it will support your body well and fit your needs. However, more expensive doesn’t always mean better – find one that suits you.
If your hips are much larger than your waist and you are a side sleeper, a firm mattress will hike one side of your hip upwards, bending your spine to one side, likely causing a stiff back the next day or worse sleep disturbances. A softer mattress will allow your hips to sink into the bed, keeping your spine straighter and limiting the strain. Likewise, if you have fairly narrow hips and wider shoulders, then a soft mattress will exaggerate this, causing your already narrow hips to sink into the mattress, once again bending your spine. For soft mattresses, you can buy firm mattress toppers and vice versa.
Sleep masks
For many with hypermobility and EDS, sleep masks are often reported to be one of the best purchases for helping with sleep. A sleep mask has been widely reported to provide relaxing sensory input and lead to better sleep. For Patients in coronary care, sleep masks were found to be very effective in improving overall sleep quality. Likewise, using a mask may help you to spend more time in REM sleep. I am fairly biased regarding sleep masks, having used one for around 2 years. As a light sleeper, I find that using a mask to block out light at night directly leads to a better night’s sleep. But, sleep masks are more of a personal preference; for every person who swears by them, there is a score who does not. Sleep masks are inexpensive these days; they come in different fabrics and weights, so they are easy to try. If sleep masks aren’t your thing, many people prefer black-out blinds.
Sex and sleep
It’s old adage that men fall asleep after sex, however, emerging research shows that it may be women who experience greater sedative properties from night sex (14). In one of these studies it states;
“Having sex while laying down with the man on top brings the female reproductive tract back into a more primate parallel orientation with gravity, and women that remain in a spline position after sex would, therefore, have a greater chance of getting pregnant. Consistent with this analysis, we found that women were unwittingly more likely to fall asleep after sex than men.”
Whilst sex does release a cascade of feel-good chemicals, increases in prolactin in men, making them more sleepy, and increases in estrogen in women, helping with REM sleep, this all likely goes much deeper than just chemicals. Feelings of intimacy and safety are a surefire way to relax and fall asleep. However, this is somewhat of a chicken and egg scenario, as poor sleep affects libido. But there is a good link between sex and sleep.
Winding down on a night
It is important for us to wind down from busy days and to prepare the body for sleep. Your body’s circadian rhythm is what is responsible for sending signals to your brain that it’s time to sleep, so regulating it properly can work wonders. Try limiting your screen time before bed, establishing a relaxing nighttime routine, and getting proper movement throughout the day. A simple walk in the morning can help regulate your body’s circadian rhythm, too!
You have likely heard this one a million times, but putting it into practice takes serious effort. Numerous glasses block blue light, claiming to help you get to sleep quicker and for better sleep. However, the evidence behind using these glasses for sleep is very wanting. At the moment, these claims don’t hold up. There are, of course, people who swear they work. This is likely a placebo, but it may be worth at least trying, if nothing else. The worst-case scenario is the glasses don’t do anything; the best case is that they do and they help you.lf tried these glasses and they did absolutely nothing, however, they did lessen the premonitory urge that companies my Tourette syndrome, so at least I got something out of their use.
Food and drink
Nothing will cause sleep disturbances as much as a full stomach while trying to sleep. The last thing your body needs while trying to wind down and fall asleep is to still be digesting food. We already established that GERD is pretty common in those with hypermobility, and late-night eating is most likely going to make this worse and lead to sleep disturbances. Trying to avoid eating 3-4 hours before bed, will at least give your body a chance to digest some of it and take the strain off of your sleep. The same is true of water before bed; instead of drinking large glasses, you could try to sip water instead.
The right pillow
This tip feels more like common sense than a tip, but it’s still worth mentioning. Again, just like mattresses, the height and firmness of your pillow should be determined by your shoulder width and sleep position. If you are a side sleeper with large shoulders, then too small of a pillow will crick your neck, likewise, too large for narrow shoulders will also have the same effect. If you are more of a sleep-on-your-back kind of person, then your pillow height won’t need to be as thick as a side sleeper. But the overarching takeaway is that you need your spine straight to take unnecessary pressure off it.
Additionally, many people with EDS/hypermobility disorders swear by finding a good body pillow or U-shaped pillow that is commonly used by pregnant people. These types of pillows, when used correctly, can help reduce pressure on certain areas of the body, alleviate pain and allow your body to fully relax. A largeu-shapede pillow allows you to place the lower section of it between your knees, keeping your hips supported, but also, as it wraps around your body, it stops you from moving too much at night and pulling your joints out of position.
Anxiety about going to sleep
It’s fairly well established that a very high percentage of those with hypermobility and Ehlers-Danloss syndrome struggle with anxiety. When you add a lack of sleep into the mix, the result can be catastrophic!
A lot of this anxiety can often be around getting to sleep. Many with hypermobility dreaded going to bed because they know they will be lying awake for many hours. I myself was in this same category for many years. I would find that as soon as I got into bed, my brain would wake up, and thoughts would fire away. I would lie trying to sleep and suddenly wonder what Jack Nickolson was in the last film. Then I would google it and find the answer, and a new thought would hit my mind. This in itself is incredibly frustrating. From working with hundreds of people with hypermobility over the years, I knew I was not alone!
One tip I will give you to help with this, and there is some research around it but nothing fantastic, is to use audio. I do not know whether listening to a podcast or an audiobook elicits the same feelings of safety I had when my mother read me bedtime stories as a kid. I do not know if it just bores my brain to sleep, but what I do know is that for myself and many others, audio helps us fall asleep.
I switched long ago from the narrative that when I go to bed, I must sleep. This narrative just causes more anxiety. What I do now when I go to bed is to go to bed knowing I am going to listen to my audiobook. By doing this, I take away the pressure that I must go to sleep. It also gives me something to focus my attention on instead of battling my thoughts.
I do the same thing every night. I set the sleep timer on audible for an hour, which means it will automatically stop playing. My sleep mask has two very thin Bluetooth speakers inside that go over my ears, so I don’t wear traditional headphones. This sleep setup works wonders for me; I always fall asleep within an hour.
Podcasts and stand-up comedy are other great audio to listen to. Now, this may not be for everyone, but if you haven’t tried it, I would recommend it. At worst, it doesn’t help, and at best, it helps you massively.
It’s Time to Invest in Your Sleep
I truly believe all people should invest in three things: their health, their happiness, and their sleep.
Ideally, humans should spend about 1/3 of their day sleeping, and when that much of your day is filled with frustration, fatigue, and restlessness, things can feel hopeless. However, taking the time to work on your sleep will help improve your physical and mental health.
When navigating life with EDS or Hypermobility Syndrome, hacking your sleep schedule is especially important to give your body time to rest and repair. It may take some trial and error to figure out what works best for you and your body, but once you start feeling rested, all the time and energy you spent trying to get a better night’s sleep will be worth it.
— Adam —
Enjoying Our Resources? Why Stop Here?
If you’ve found value in our posts, imagine what you’ll gain from a structured, science-backed course designed just for you. Hypermobility 101is your ultimate starting point for building strength, stability, and confidence in your body.
FAQ: Common Questions About EDS and Sleep
A number of interrelated factors contribute to the difficulty with sleep experienced by individuals with Ehlers-Danlos Syndrome (EDS). Finding a comfortable sleeping position becomes a challenge for those with chronic pain and discomfort caused by joint instability. Additionally, hypermobility increases the risk of painful dislocations while you sleep. Problems with the nervous system, including memory loss and chronic headaches, can make it even more difficult to fall or stay asleep. Many individuals with EDS also suffer from autonomic dysfunction, which can lead to sleep disorders like obstructive sleep apnoea, which disrupts breathing while you’re asleep. The quality of one’s sleep can also be affected by psychological factors, such as anxiety and depression. Finally, a vicious cycle of poor sleep followed by increased tiredness is created by the chronic fatigue that is associated with EDS. Medical management and individualised support are often necessary components of a holistic strategy for overcoming these obstacles.
It is true that heat can worsen symptoms for people with Ehlers-Danlos Syndrome (EDS), especially for hypermobile EDS (hEDS). Hot weather can make people more sensitive to pain, which in turn can amplify symptoms like muscle fatigue and joint pain. Symptoms like vertigo and rapid heartbeat, brought on by dysautonomia, can become more severe in hot environments for people with hEDS. Heat also increases tiredness and skin reactions, making everyday tasks more difficult. Staying hydrated, avoiding strenuous activities in the heat, and using cooling methods to effectively regulate body temperature are recommended ways to manage these effects. Evidence from studies showing that hEDS symptoms are similar to those of disorders like fibromyalgia, which can also be made worse by heat, corroborate these findings
It is crucial to prioritise support, pressure relief, and adjustability when choosing a pillow for individuals with Ehlers-Danlos Syndrome (EDS) and hypermobility. If you sleep on your side, use a body pillow like the Pharmedoc U-Shape Pregnancy Pillow; if you suffer from joint pain, try a wedge pillow like the Kölbs Bed Wedge Pillow; and if you’re a memory foam pillow fan, try the Tempur Cloud Comfort Pillow. The Mediflow Water Pillow is one example of an adjustable water pillow; cervical pillows aid in keeping the neck in a neutral position while you sleep. Feel free to try out various combinations of these pillows to find the perfect fit for your comfort and support needs. If you want expert advice, it’s best to consult a healthcare professional.
Although people with hypermobility or Ehlers-Danlos Syndrome (EDS) may not necessarily require more sleep, the necessity for restorative sleep is greatly amplified in cases of chronic pain. Daytime weariness and an increased perception of the need for sleep are consequences of pain’s disruption of sleep cycles, which prevents deep, restorative sleep and causes frequent awakenings. A vicious cycle is formed when pain and sleep deprivation feed into one another, as poor sleep further reduces pain tolerance and amplifies discomfort. Even though people get the recommended amount of sleep each night, they may still feel exhausted if they suffer from comorbid conditions such as autonomic dysfunction or obstructive sleep apnoea (OSA). Better pain management, treatment of underlying sleep disorders, and optimisation of sleep hygiene can all contribute to better sleep quality rather than more sleep overall.
Chronic pain from unstable joints and myofascial tension directly interferes with sleep architecture. Disrupted sleep further lowers pain thresholds through altered cytokine profiles (e.g., IL-6 elevation) and central sensitization710. A study of hemodialysis patients—a population with overlapping sleep-pain comorbidities—found that structured stretching reduced pain-related sleep interruptions by 34%
References:
1) Andersen, M.L., Araujo, P., Frange, C. and Tufik, S. (2018). Sleep Disturbance and Pain. Chest, 154(5), pp.1249–1259. doi:https://doi.org/10.1016/j.chest.2018.07.019.
2) Gerhart, J.I., Burns, J.W., Post, K.M., Smith, D.A., Porter, L.S., Burgess, H.J., Schuster, E., Buvanendran, A., Fras, A.M. and Keefe, F.J. (2016). Relationships Between Sleep Quality and Pain-Related Factors for People with Chronic Low Back Pain: Tests of Reciprocal and Time of Day Effects. Annals of Behavioral Medicine, [online] 51(3), pp.365–375. doi:https://doi.org/10.1007/s12160-016-9860-2.
3) Finan, P.H., Goodin, B.R. and Smith, M.T. (2013). The Association of Sleep and Pain: An Update and a Path Forward. The Journal of Pain, [online] 14(12), pp.1539–1552. doi:https://doi.org/10.1016/j.jpain.2013.08.007.
4) Verbraecken, J., Declerck, A., Van de Heyning, P., De Backer, W. and Wouters, E. (2002). Evaluation for sleep apnea in patients with Ehlers-Danlos syndrome and Marfan: a questionnaire study. Clinical Genetics, 60(5), pp.360–365. doi:https://doi.org/10.1034/j.1399-0004.2001.600507.x.
5)Benson, K. (2019). Are We ‘Brain Washed’ during Sleep? [online] Boston University. Available at: https://www.bu.edu/articles/2019/cerebrospinal-fluid-washing-in-brain-during-sleep/.
6) Ma, Y., Liang, L., Zheng, F., Shi, L., Zhong, B. and Xie, W. (2020). Association Between Sleep Duration and Cognitive Decline. JAMA Network Open, [online] 3(9), p.e2013573. doi:https://doi.org/10.1001/jamanetworkopen.2020.13573.
7) Vikesh Khanijow, Prakash, P., Emsellem, H.A., Borum, M.L. and Doman, D.B. (2015). Sleep Dysfunction and Gastrointestinal Diseases. Gastroenterology & Hepatology, [online] 11(12), p.817. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC4849511/.
8) Tapasak, B.E. and Malis, D.J. (2022). The Mystery of Ehlers-Danlos Syndrome: An Autobiographical Case Report. Cureus, [online] 14(1), p.e21601. doi:https://doi.org/10.7759/cureus.21601.
9) Anna S. Stöberl, Gaisl, T., Giunta, C., Noriane A. Sievi, Singer, F., Möller, A., Rohrbach, M. and Kohler, M. (2018). Obstructive Sleep Apnoea in Children and Adolescents with Ehlers-Danlos Syndrome. Respiration, 97(4), pp.284–291. doi:https://doi.org/10.1159/000494328.
10) Gaisl, T., Giunta, C., Bratton, D.J., Sutherland, K., Schlatzer, C., Sievi, N., Franzen, D., Cistulli, P.A., Rohrbach, M. and Kohler, M. (2017). Obstructive sleep apnoea and quality of life in Ehlers-Danlos syndrome: a parallel cohort study. Thorax, [online] 72(8), pp.729–735. doi:https://doi.org/10.1136/thoraxjnl-2016-209560.
11) Kaltenbach, T., Crockett, S. and Gerson, L.B. (2006). Are Lifestyle Measures Effective in Patients With Gastroesophageal Reflux Disease? Archives of Internal Medicine, 166(9), p.965. doi:https://doi.org/10.1001/archinte.166.9.965.
12) Lee, H., Xie, L., Yu, M., Kang, H., Feng, T., Deane, R., Logan, J., Nedergaard, M. and Benveniste, H. (2015). The Effect of Body Posture on Brain Glymphatic Transport. Journal of Neuroscience, 35(31), pp.11034–11044. doi:https://doi.org/10.1523/jneurosci.1625-15.2015.
13) Kim, W.Y., Hong, S.-N., Yang, S.K., Nam, K.J., Lim, K.H., Hwang, S.J., Seo, M.Y. and Lee, S.H. (2019). The effect of body position on airway patency in obstructive sleep apnea: CT imaging analysis. Sleep and Breathing, 23(3), pp.911–916. doi:https://doi.org/10.1007/s11325-019-01863-x.
14) Apa.org. (2025). APA PsycNet. [online] Available at: https://psycnet.apa.org/record/2020-13738-001 [Accessed 27 Feb. 2025].